
 Dementia
Dementia
Headlines
- Dementia accounts for more years of disability than any other condition.
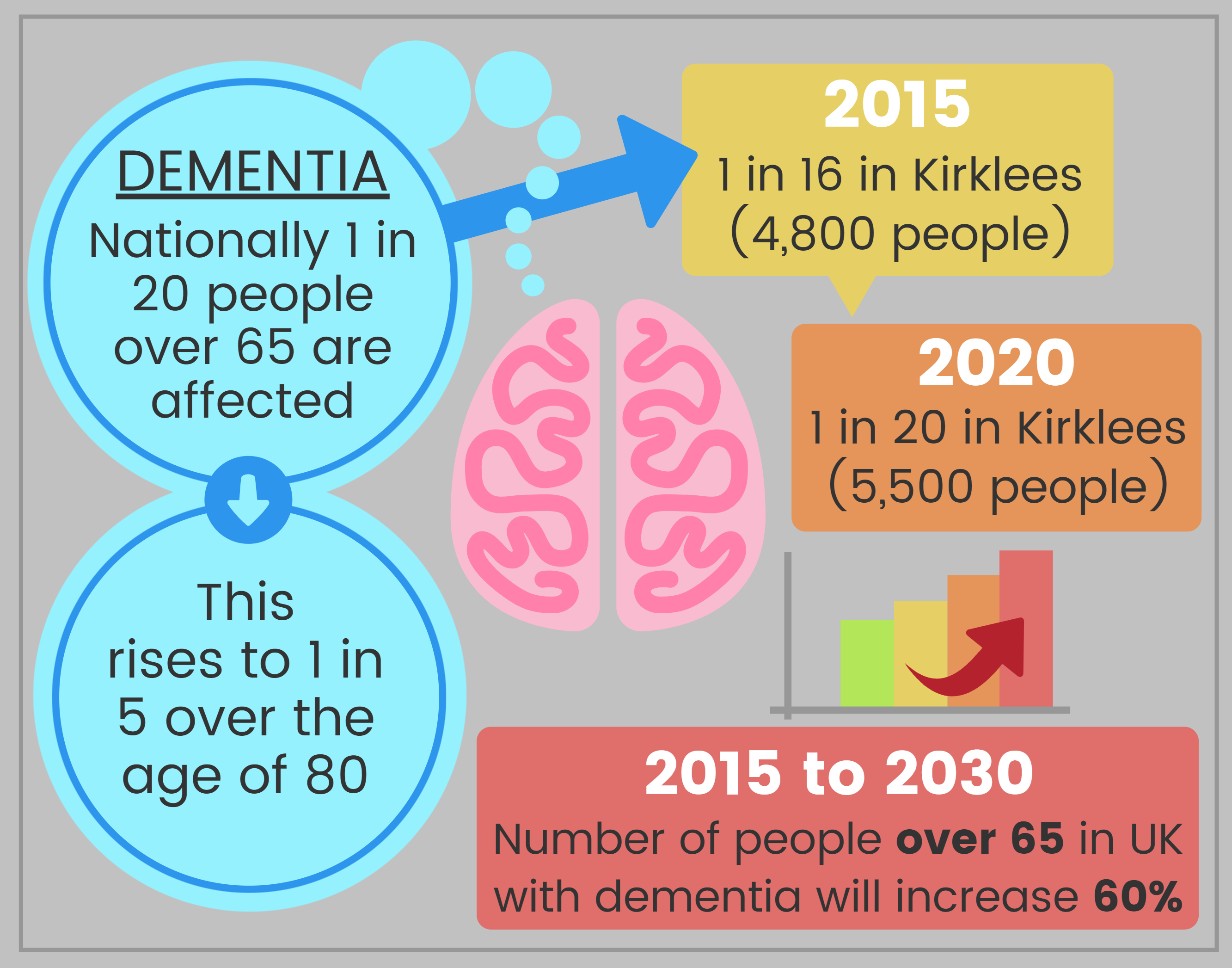
- In Kirklees it is estimated that nearly 1 in 16 (4,800) people aged over 65 had dementia in 2015, and that this is projected to rise to nearly 5,500 or 1 in 14 by 2020. There are also estimated to be just over 100 people under 65 with early onset dementia.
- Cases of dementia are expected to double by 2030.
- Dementia increases rapidly with age. 10% of deaths in men aged over 65 years and 15% in women aged over 65 years are attributable to dementia.
- Nationally only 1 in 3 people with dementia ever receive a formal diagnosis or have contact with specialist services at any time in their illness. In Kirklees almost half of people predicted to have dementia are known to services.
- Dementia is caused by a number of conditions including vascular disease so is directly affected by lifestyle behaviours.
- People with Down’s syndrome are four times more likely to develop dementia and for it to begin at an earlier age.
- 2 in 3 people with dementia are cared for in the community, mostly by unpaid carers; the rest live in care homes.
- There is a shortage of good quality dementia nursing care locally.
Why is this issue important?
The term ‘dementia’ is used to describe a set of symptoms which result from the ongoing deterioration of the brain, caused by a number of diseases in which there is a progressive decline in multiple areas of function, including memory, reasoning, communication skills and the ability to carry out daily activities. There are individual differences in the speed and progression of dementia; people may live with it for up to 15 years after diagnosis, but it is a terminal illness. Each person is unique and will experience dementia differently (1).
The symptoms of dementia (2) include:
- Poor concentration.
- Memory loss, for example names of people and places, events that have taken place.
- Extreme tiredness.
- Asking the same questions repeatedly.
- Mood swings or aggressive behaviour.
- Confusion about the time of day.
- Losing things or putting things in inappropriate places.
- Getting lost in previously familiar places.
- Difficulties understanding people and finding the right words.
10% of deaths in men aged over 65 years, and 15% of deaths in women aged over 65 years are attributable to dementia. Delaying the onset of dementia by five years would reduce the number of UK deaths due to dementia by 30,000 per year (3).
Generally, only 1 in 3 people nationally with dementia ever receive a formal diagnosis or have contact with specialist services at any time in their illness. However diagnosis rates have improved in Kirklees and now almost half of people predicted to have dementia have a diagnosis and are known to services (2).
Nationally, it is estimated that 1 in 20 people over the age of 65 years are affected by dementia and 1 in 5 people aged over 80 years. By 2030 it is estimated that this will have increased by more than 60%. In Kirklees it is estimated that nearly 1 in 16 (4,800) people aged over 65 had dementia in 2015, and that this is projected to rise to nearly 5,500 or 1 in 14 by 2020 (4).
It is estimated that there are over 100 people locally with young onset dementia, i.e. aged under 65 years, and this is expected to increase slightly to around 110 by 2020.
What significant factors are affecting this issue?
Increasingly, age is the main risk factor but other factors include genetic background, medical history and health behaviours. About half of all cases of dementia have a vascular component (i.e. linked to the blood supply to the brain) and so are linked to smoking, diet and physical activity (3).
Risk of dementia may be reduced by adopting positive health behaviours such as eating a healthy diet, not smoking, being physically active, drinking less alcohol and protecting the brain from injury (5).

- Good nutrition contributes to healthy brain development, which may protect against the onset of dementia in late life.
- Obesity in midlife and diets rich in saturated fat, which predispose to cardiovascular disease, may increase the risk of developing dementia in late life.
- Maintaining an adequate diet is challenging for people with dementia, leading to a particularly high prevalence of under nutrition – training to care givers and care home staff to raise awareness that people with dementia take longer to eat, require prompting and encouragement and may have problems with coordination and swallowing.
- Early intervention to improve awareness of the importance of a balanced diet, including strategies to boost the energy content of the diet may help to prevent or delay the complications of long-term inadequate food intake.
An increase in the population aged over 65 years, particularly those aged over 85 years, is likely to lead to an increase in the numbers of people with dementia. This will also increase the demand for health and social care services, especially as there will be proportionately fewer young people and family networks available to provide unpaid care.
Up to half of all people with dementia also have depression. People with both dementia and depression have higher rates of disability and higher rates of hospital admission than people with dementia alone (6).
Dying with Dementia
- Dementia and Alzheimer disease accounted for 11.6% of deaths registered in England and Wales in 2015 (7).
- Nationally two-thirds of people say they would prefer to die at home.
- The majority (58%) of deaths with a mention of dementia occurred in care homes. By comparison a much lower proportion (25%) of all deaths in the general population aged 65+ happen in a care home setting.
- Only 8% of people who die with dementia pass away at home, compared to 21% of the general population aged 65+. They are less likely to die at home than people dying with cancer, circulatory or respiratory diseases.
- Nearly a third (32%) of people who die with a mention of dementia die at a hospital, a lower proportion than in the general population (49%) or amongst those dying with cancer, circulatory or respiratory diseases.
- Only 1% of deaths with dementia happen in a hospice, compared with 5% of deaths in the general population aged 65+. People with dementia are less likely to die in a hospice than people dying of cancer.
- People who die with dementia are more likely to die younger if they reside in more deprived areas. The proportion difference is small but significant and is more pronounced for people with vascular dementia.
End of life care can pose difficulties because dementia is not always predictable. Ideally, patients with dementia should be asked about their end of life wishes before they lose capacity, but these are not easy conversations. Relatives and carers continue to have a very important role if a patient is in hospital or has gone into care and need to be listened to carefully. Relationships between relatives and professional carers can quite easily become fraught. An end of life plan, incorporating the known wishes of the patient, is especially helpful if relatives disagree among themselves about how much intervention should occur in the event of deterioration (8).
Which groups are most affected by this issue?
Some population groups are more likely to develop dementia (2):
- Generally people from minority ethnic groups experience higher rates of young onset dementia and vascular dementia than the white population.
- More women have dementia.
- People with Down’s syndrome are four times more likely to develop dementia and for it to begin at an earlier age.
Where is this causing greatest concern?
The highest rate of dementia diagnosis in those aged over 65 years in Kirklees was in North Kirklees, but variation across Kirklees was very small; this also only represents those known to services (9).
What are the assets around this issue?
Health assets are those things that enhance the ability of individuals, communities and populations to maintain and sustain health and well-being. These include things like skills, capacity, knowledge, networks and connections, the effectiveness of groups and organisations and local physical and economic resources. They also include services or interventions that are already being provided or beginning to emerge which contribute to improved health and wellbeing outcomes.
Assets are hugely important to how we feel about ourselves, the strength of our social and community connections and how these shape our health and wellbeing.
As part of our KJSA development we are piloting a range of methods to capture and understand the assets that are active in Kirklees. Please see the assets overview section for more information about our approach and if you are interested in place-based information about assets in Kirklees have a look at the assets section in each of our District Committee summaries (Batley and Spen, Dewsbury and Mirfield, Huddersfield and Kirklees Rural). Where possible and appropriate we will provide information about local assets supporting people across different stages of the life course.
The council has commissioned Making Space to deliver the Kirklees Dementia Information Service to provide comprehensive information about services available within Kirklees and appropriate signposting support to People with Dementia, their Carers and Family Members to facilitate easier and earlier access to a full range of generic and specialist services at all points during their journey. There are many local dementia support groups and services available in both North and South Kirklees from befriending and dancing to lunch clubs and exercise classes. The Dementia Practitioner’s Forum meets regularly with representatives from many of the support groups attending to discuss.
Kirklees has an active Kirklees Dementia Action Alliance (KDAA) which has almost 200 members. To make Kirklees Dementia Friendly, we need to continue to increase the number of dementia friends across the district. Training sessions can be provided by the alliance to businesses, schools and community groups.
Views of local people
Focus groups with local people aged over 65 years (6) to understand perceptions of dementia highlighted:
- People reported very little awareness of dementia until someone close to them is diagnosed. Getting an early diagnosis is important to people, it reduces anxiety and worry.
- The amount of information available can be overwhelming and people don’t know what to ask for and when.
- End of life /advanced directives don’t appear to be routinely discussed.
Also see reference (2).
What could commissioners and service planners consider?
Commissioners, service planners and Councillors should consider local community assets such as those outlined above so that they can support and build on local strengths and also understand where there are gaps and unmet needs in particular places or amongst particular communities.
Other items of consideration should include:
- Raising public awareness about dementia, reducing the stigma and fear associated with dementia, raising awareness of the modifiable risk factors and encouraging people to seek help and obtain a diagnosis
- Focusing on prevention and encouraging or enabling people to behave in ways which will improve their health outcomes (for example, relating to heart disease and stroke which increase the risk of vascular dementia) to reduce those risk factors associated with some dementias which we can do something about, e.g. alcohol use.
- Conduct focused efforts to reduce alcohol abuse in order to prevent or reduce alcohol related dementias such as Korsokoff Syndrome.
- Focus on improving the diagnosis of dementia, as early as possible.
- Provide improved support for carers.
- Develop more flexible housing/accommodation options which should include:
- More support for people to remain safely at home.
- Good quality residential and nursing care places.
- Increasing the range of accommodation choices for people with dementia, including extra care schemes.
- Influencing the design of accommodation to create environments which provide stimulation, enjoyment and dignified person-centred care.
- Improve the provision of intermediate care and rehabilitation to reduce unnecessary or prolonged hospitalisation.
- Discussions around End of Life should become part of normal conversation. There are taboos that need to be addressed if people with dementia are to have their end of life wishes acknowledged and acted upon.
- Promote the use of the Kirklees online platform ‘My Health Tools’ (www.myhealthtools.uk) to help people living with long term health conditions to find information, resources and support.
Further information will be found in the Kirklees Dementia Needs Assessment.
References and additional resources/links
- Alzheimer’s Society. What is Alzheimer’s disease? [Internet]. 2016. Available from: https://www.alzheimers.org.uk/site/scripts/documents_info.php?documentID=100
- NHS, Kirklees Council. Living Life to the Full. Living with Dementia in Kirklees [Internet]. 2016. Available from: http://www.kirklees.gov.uk/beta/health-and-well-being/pdf/living-with-dementia.pdf
- Department of Health. Prime Minister’s challenge on dementia 2020 [Internet]. 2015. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/414344/pm-dementia2020.pdf
- Projecting Older People Population Information (POPPI) [Internet]. [cited 2016 Oct 3]. Available from: http://www.poppi.org.uk/
- Alzheimer’s Society. Advice for nurses and other healthcare professionals [Internet]. 2016. Available from: https://www.alzheimers.org.uk/site/scripts/documents_info.php?documentID=1211&pageNumber=3
- Department of Health. Dementia. A state of the nation report on dementia care and support in England [Internet]. 2013. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/262139/Dementia.pdf
- Office for National Statistics. Deaths registered in England and Wales (Series DR): 2015 [Internet]. 2016. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsregisteredinenglandandwalesseriesdr/2015#dementia-and-alzheimer-disease-was-the-leading-cause-of-death-in-2015
- Public Health England. Dying with dementia [Internet]. 2016. Available from: http://www.yhpho.org.uk/resource/view.aspx?RID=237877
- NHS Digital. Quality Outcomes Framework (QOF) Recorded Dementia Diagnoses [Internet]. 2016 [cited 2016 Oct 3]. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/recorded-dementia-diagnoses/qof-april-2014-january-2015
The Kirklees Dementia Needs Assessment can be found here:
http://www.kirklees.gov.uk/beta/adult-social-care-providers/pdf/kirklees-dementia-needs-assessment.pdf.
My Health Tools: www.myhealthtools.uk
Date this section was last reviewed
18/11/16 (Dementia Needs Assessment link amended 16/03/17)
