![]()
 Sexual Health
Sexual Health
Headlines
Why is this issue important?
Anyone who is sexually active can contract sexually transmitted infections (STIs). People are at greater risk if they have casual partners, change partners frequently, do not have regular full STI screens or don’t use an appropriate barrier method when having sexual contact (i.e. male condom, receptive condom or dental dam).
- Many STIs do not show symptoms meaning they can be difficult to diagnose and so remain untreated.
- Untreated infections increase the risk of onward infection and the spread of infections.
- If left untreated, STIs can have serious long-term health consequences and some can be life-threatening.
- Infertility can be the result of STIs in both males and females.
- Some STIs can be passed from mother to child during pregnancy and birth.
- Untreated syphilis can lead to damage to the heart, respiratory system and nervous system, and cause disabilities in new-born babies.
- HIV is still an incurable infection that will need to be medically managed for the duration of the sufferer’s lifetime. Where it is diagnosed late it is likely to significantly reduce life expectancy and be more costly to the NHS and Local Authorities; the costs of HIV care remains 50% higher for each year after diagnosis if the diagnosis is late.(1)
All STIs are preventable through safe sex behaviours. The effective communication of easy to understand safe sex messages is therefore paramount. Reducing the transmission of STIs requires early detection, successful treatment and partner notification alongside promotion of safer sexual behaviour and the use of sexual healthcare services.
What significant factors affect this issue?
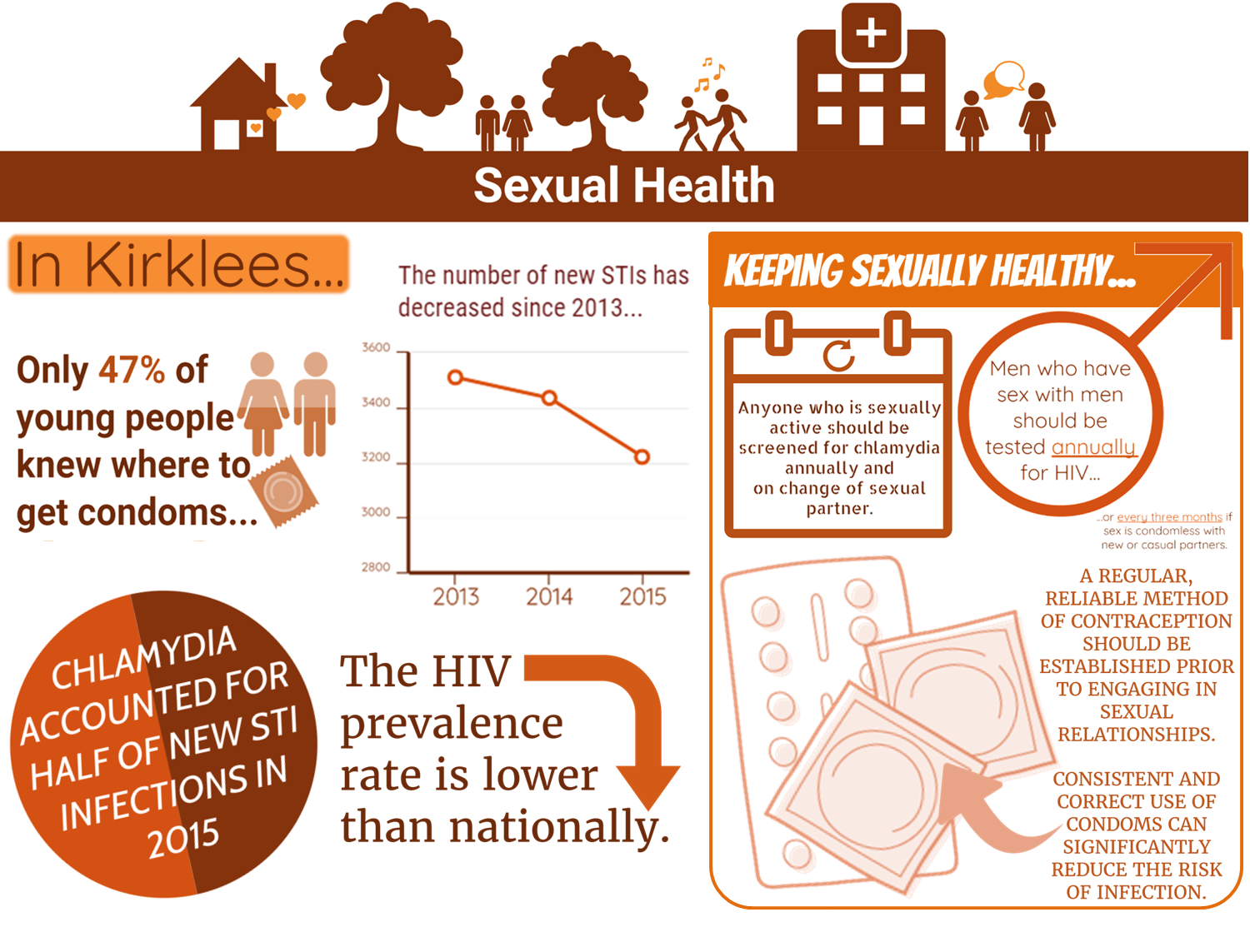
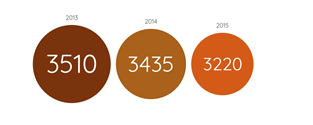
The most common STIs are chlamydia, genital warts, genital herpes, gonorrhoea and syphilis. In Kirklees, the total new cases of STIs have decreased gradually since 2013 (2):
Incidences of STIs are likely to be explained by several reasons including:
Risky behaviours
Alcohol intoxication is associated with an increased risk that people will have unprotected sex. Failure to use a condom during a young person’s first sexual encounter is linked to alcohol consumption.(3)
Awareness
Myths about sex, fertility and abortion still exist and awareness of the full range of contraception is low. This may be linked to inconsistent sex and relationships education (SRE) in schools.
At home a significant number of parents lack the knowledge and/or confidence to talk to their children about sex and relationships. In addition the wider children’s workforce is not routinely equipped to talk to young people about their relationships and their sexual health.
Increased awareness is also needed in older age groups, particularly around the need for regular testing, which could help with the late diagnosis of some infections.
Regular screening
Sexually active individuals should get a full STI screen regularly, particularly when they change partners or if they have casual partners.
Accessibility of services
Sexual health services should be convenient and accessible and in a setting which is acceptable to the individual, particularly those who are vulnerable or at increased risk.
Partner notification
Sexual health services should advocate partner notification to prevent the spread of infection.
What does the local data tell us?
Despite the decline in total numbers, there continue to be issues of concern in Kirklees:
- Chlamydia accounted for half of all new STI infections locally in 2015.(2)
- Chlamydia is very often asymptomatic so a high screening rate is necessary to detect infections. In Kirklees 18.9% of 15-24 years olds were tested for chlamydia which was significantly lower than nationally (22.5%).(4)
- Kirklees has an annual chlamydia diagnosis rate (in 15-24 year olds) of 2,031 per 100,000 which is lower, but not significantly, than the rate recommended by Public Health England (2,300 per 100,000).(4)
- Of those tested, 10.7% received a positive result. This was significantly higher than nationally (8.4%). This suggests that despite a lower screening rate, services are relatively good at targeting people at higher risk of infection. Of the 21 local authorities in the Yorkshire and Humber region, Kirklees has the 10th highest rate of diagnosis.(2)
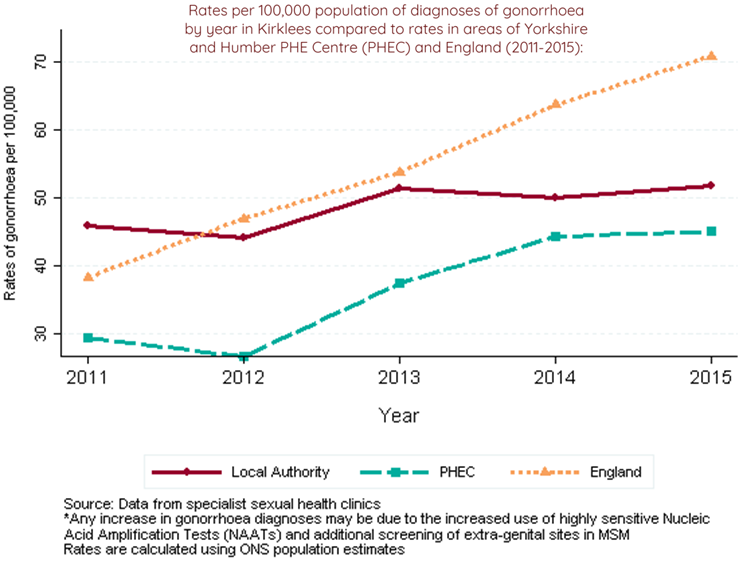
- Gonorrhoea has steadily increased from 2009 (28.0 per 100,000). In 2015, the rate of diagnoses was 51.7 per 100,000.(4) The upward trend is of concern particularly in the context of antibiotic resistance in gonorrhoea infections.
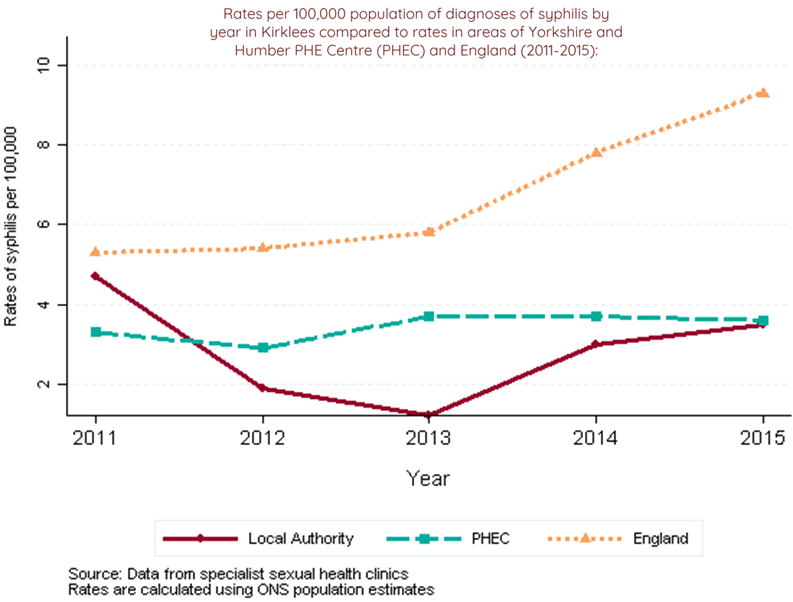
- There has been an overall decline in the diagnosis rate for syphilis in Kirklees between 2009 and 2015, although there was an approximate three-fold increase in cases between 2013 and 2014. After this point the figure has stabilised and was significantly lower than the national rate; 3.5 per 100,000 in 2015 compared to 9.3 nationally. Kirklees ranks 173rd out of 326 authorities in England for rates of syphilis (where 1st has the highest rate).(2)
- In Kirklees in 2015, the diagnosed prevalence rate for HIV in people aged 15-59 years old was significantly lower than nationally (1.4 per 1000 compared with 2.3 per 1000).(4)
- In Kirklees, between 2013 and 2015, 48.3% of HIV diagnoses were made at a late stage of infection compared to 40.3% in England.(4)
- In Kirklees in 2015, 73.6% of eligible patients at specialist sexual health clinics were tested for HIV. This compares to an equivalent figure nationally of 67.3%.(2)
- The total numbers of new diagnoses of HIV have stabilised but with effective treatments now available, the numbers of people living with and accessing care for HIV increases year on year.
Which groups are affected most by this issue?
- Overall, of those diagnosed with a new STI in Kirklees in 2015, 46% were male and 54% were female.(2)
- Young people aged between 15 and 24 years old experience the highest rates of new STIs. In Kirklees, 54% of diagnoses of new STIs made in specialist sexual health clinics were in young people aged 15-24 years.(2)
- Young people are also more likely to become re-infected with STIs. In Kirklees an estimated 13% of 15-19 year old females and 12.2% 15-19 year old males present with a new STI at a specialist clinic during the period 2011 to 2015 were re-infected within 12 months.(2)
- Reinfection with an STI is an indicator of persistent risky behaviour. In Kirklees, an estimated 8.2% of males and 8.3% of females presenting with a new STI at a specialist sexual health clinic between 2011 and 2015 became re-infected with a new STI within 12 months. Nationally the figures were 9.3% and 7.1% respectively.(2)
- Older age groups were most affected for some specific infections, notably syphilis, which mainly affected the 35-45 year old age group.(2
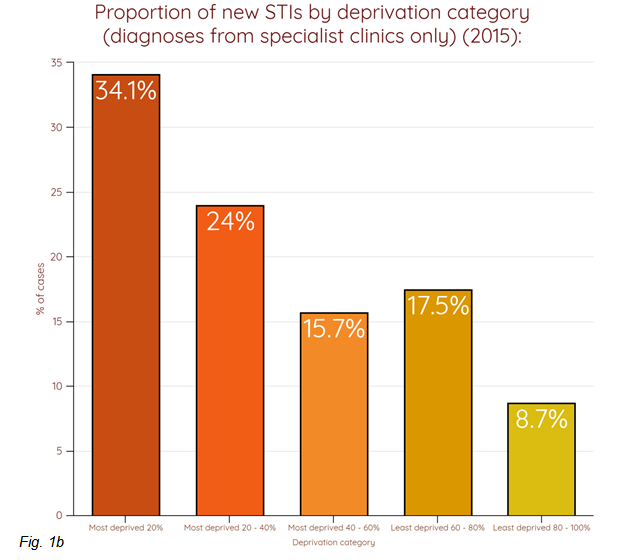
- Across all age groups, almost twice as many people diagnosed with an acute STI were from the most deprived population group compared to the least deprived.(2)
- In Kirklees in 2015, around twice as many males as females received HIV-related care.(2)
- In relation to exposure, about 40% probably acquired HIV through sex between males and 53% through sex between males and females.(2)
- The populations known to be at risk of difficulty accessing routine contraception include teenagers, NEET young people, the homeless, asylum seekers and refugees, those with mental health problems, young offenders and females involved in the criminal justice system and victims of sexual violence, and those suffering domestic abuse from alcohol and drug problems.
Where is this causing greatest concern?
The 2014 Kirklees Children and Young People’s survey (5) provides information on sexual activity amongst this group. The survey identified:
- The District Committees with slightly higher overall levels of Year 9s who said that they had had sex were Batley and Spen and Kirklees Rural (8%) (compared to Dewsbury and Mirfield and Huddersfield (6%).
- These areas also had a more pronounced difference between genders. In Batley and Spen 11% of Year 9 females said they had had sex (compared with 5% of males) and in Kirklees Rural, 10% of Year 9 males said they had had sex (compared with 6% of females).
- For all year 9s, the lowest rate of any reported sexual intercourse was in Huddersfield (7%) and the highest was in Kirklees Rural (13%).
- Out of all respondents in Years 9 and 12 who said they were sexually active, 30% overall said that they never use a condom. This proportion was highest in Batley and Spen (42%) and lowest in Kirklees Rural (13%).
- Overall 47% knew where to get condoms (the lowest proportion (39%) of young people who knew where to go was in Dewsbury and Mirfield).
- Batley and Spen had a higher proportion of young people who reported having sex after consuming alcohol (62%; all other District Committees were around 47%).
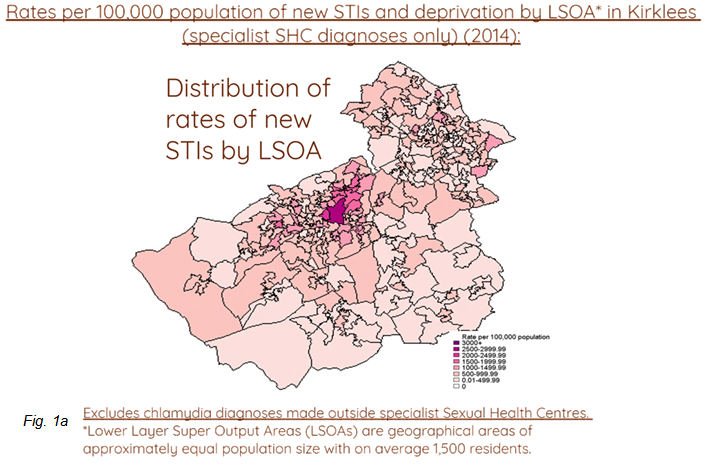
- There is also a strong link between rates of new STIs and levels of deprivation. This relationship is probably related to a range of factors including poorer access to health services, education and health awareness. This is highlighted in Figure 1a and 1b (2):
What are the assets around the issue?
Health assets are those things that enhance the ability of individuals, communities and populations to maintain and sustain health and well-being. These include things like skills, capacity, knowledge, networks and connections, the effectiveness of groups and organisations and local physical and economic resources. They also include services or interventions that are already being provided or beginning to emerge which contribute to improved health and wellbeing outcomes.
Assets are hugely important to how we feel about ourselves, the strength of our social and community connections and how these shape our health and wellbeing.
As part of our KJSA development we are piloting a range of methods to capture and understand the assets that are active in Kirklees. Please see the assets overview section for more information about our approach and if you are interested in place-based information about assets in Kirklees have a look at the assets section in each of our District Committee summaries (Batley and Spen, Dewsbury and Mirfield, Huddersfield and Kirklees Rural). Where possible and appropriate we will provide information about local assets supporting people across different stages of the life course.
There are a number of sexual health services for people in Kirklees including the NHS, independent sector, local authority, and the voluntary sector, offering different levels of service.
A new Integrated Sexual Health Service is now in place across Kirklees which brings together services for contraception and for sexually transmitted infections. The new service has a much greater emphasis on prevention and better access for people at a higher risk of poor sexual health, offering:
-
- more intensive one-to-one support for people who return to the service re-infected with an STI within 12 months of a previous infection;
-
- an outreach programme for young people;
-
- more resources targeted at Sex and Relationships Education in schools, including direct delivery in targeted areas.
Kirklees C-Card Scheme distributes condoms free of charge to young people under 25 from a wide range of community venues such as sports clubs and youth centres. The service promotes sexual and reproductive health provides an opportunity for young people to talk about their relationships and sexuality in a safe, non-judgemental and confidential space that best suits them and with an adult they trust. C-Card interventions can also help young people find their way to other services they may need – including other health services, social care or education. The scheme also provides access to free chlamydia screening and pregnancy testing is also available at some locations.
The Brunswick Centre provides HIV Support and HIV prevention services across Kirklees. As well as advocacy, support groups and one-to-one support, the service also supplies condoms to communities at increased risk of HIV infection. The team also run a condom-by-post scheme and can anonymously mail out small quantities of condoms to Kirklees residents who require this service.
Chlamydia screening services (CHLASP) have been established in Kirklees over many years and are now part of the Integrated Service. CHLASP targets under-25s as the group most at risk of becoming infected with chlamydia.
Emergency Hormonal Contraception is available for all ages free of charge through certain pharmacies as well as GPs and sexual health services.
The Sexual Health Network brings together providers of sexual health services including the voluntary sector, commissioners of services and services that work with groups who may be at higher risk of poor sexual health. This enables local data, epidemiological and anecdotal, to be shared so that services are better able to respond to outbreaks or other changing patterns in sexual health across the district.
A multi-agency partnership has been formed to improve the response of services to meet the needs of sex workers and the communities where they work. This has representatives from sexual health services, the Police, anti-social behaviour team, social care and voluntary sector support organisations.
Schools as Community Hubs are collaborations between schools and will enable sharing of staff expertise in Sex and Relationships Education across schools.
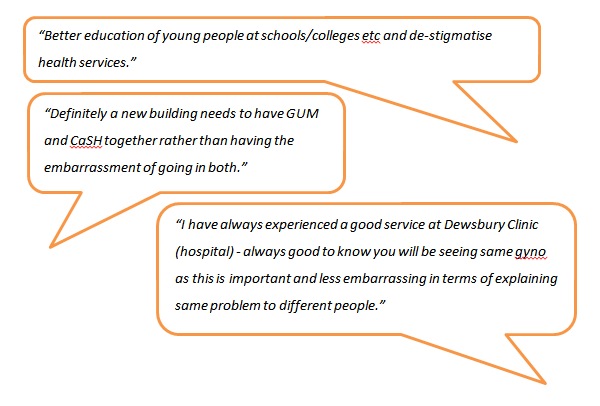
Views of Local People
The Healthwatch publication The Future of Sexual Health Services in Kirklees collated insight from local people relating to where they would like to access services, concerns over confidentiality, opinions of staff working in Sexual Health services and information they received about prevention, amongst other things:
In the near future, we will have more sources of information regarding local people’s view of sexual health including:
- A school survey run by school nurses specifically on sexual health.
- The SWEET (Sex Worker Empowerment, Education and Training) project is beginning to compile sex workers view of sexual health services.
- The Sexual Health Services are compiling views on the services in terms of sexual health provision.
What could commissioners and service planners consider?
Commissioners, service planners and Councillors should consider local community assets such as those outlined above so that they can support and build on local strengths and also understand where there are gaps and unmet needs in particular places or amongst particular communities.
Local authorities are responsible for providing comprehensive, open access sexual health services.
- All sexual health services need to be designed and provided so that they are accessible and welcoming to young people as well as the adult population.
- Greater emphasis on prevention of sexual ill health within service delivery is needed.
- The needs of the groups at highest risk of sexually transmitted infections should be identified and reflected in health improvement programmes.
- Services and organisations that work with those groups need to ensure seamless pathways are in place and that there is a high level of awareness of services available.
- Targeted prevention work in teenage pregnancy hotspots is advisable.
- There should be a more consistent approach to Sex and Relationships Education (SRE) in schools, including:
- whole school policy to include support and upskilling for staff and reducing stigma around sexual health;
- specialist support from the sexual health service to advise on content and approach of SRE;
- accessible drop-in services in schools.
- A comprehensive, multi-agency approach to workforce development and training is essential to ensure greater awareness of :
- opportunities to communicate safe sexual health messages;
- what services are available;
- the need to test and diagnose early.
- Primary care services, particularly general practice, need to be aware of the groups at highest risk as well as the signs and symptoms of HIV and STIs. This will ensure individuals are screened or referred opportunistically as appropriate.
- Testing and early diagnosis of HIV in primary care, the acute sector and in the community should be prioritised.
- Raising awareness of gonorrhoea in a targeted manner, including threat of antibiotic resistance and treatment protocols, should also be prioritised.
References
- NICE. HIV testing. Available from: https://www.nice.org.uk/advice/lgb21/chapter/costs-and-savings
- Kirklees Local Authority. HIV, sexual and reproductive health epidemiology report (LASER): 2015. 2016.
- Newbury-Birch D, Walker J, Avery L, Beyer F, Brown N, Jackson K, et al. Impact of Alcohol Consumption on Young People A Systematic Review of Published Reviews. 2009;1–66.
- Public Health England. Sexual and Reproductive Health Profiles. 2015. Available from: http://fingertips.phe.org.uk/profile/sexualhealth
- Kirklees Council. Children and Young People’s Survey 2014. 2014.
- Kirklees Council. Teenage conceptions Ward level 2012-14. 2014.
- Public Health England. Human Papillomavirus (HPV) vaccination coverage in adolescent females in England : 2014 / 15 About Public Health England. 2014; Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/412264/HPV_Vaccine_Coverage_in_England_200809_to_201314.pdf
Additional resources/links
- Locala Sexual Health Centres offer a full range of contraception, testing and treatment for STIs and chlamydia screening. Clinic times can be found here.
- Kirklees Council has an online resource detailing local screening and treatment for various STIs which can be found here.
- The Brunswick Centre runs a Kirklees “condoms by post” scheme and can anonymously mail out small quantities of condoms. Details can be found here.
- You can find details of where condoms are available for free here.
Date this section was last reviewed
01.06.17
