
 Cancer
Cancer
Headlines
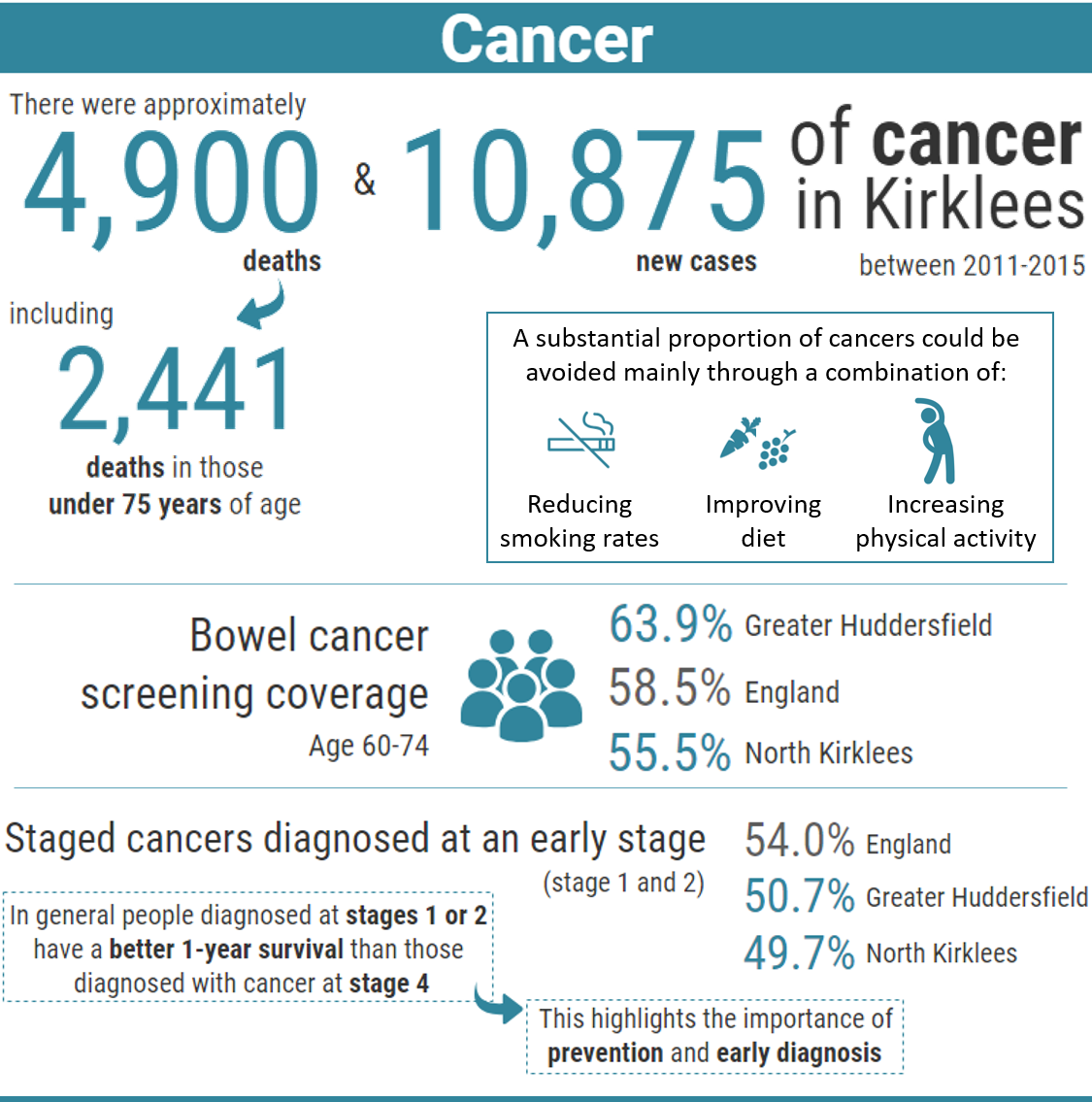
Why is this issue important?
Cancer diagnosed at a later stage is associated with worse outcomes and survival rates. With one in two people born after 1960 estimated to be diagnosed with some form of cancer during their lifetime, this highlights the importance of screening and early diagnosis of cancer. People are at greater risk if they do not attend for regular screening, are unaware of symptoms to look out for, or partake in particular lifestyle choices.
Four in ten cases of cancer could be prevented by lifestyle changes, such as not smoking, keeping a healthy body weight, cutting back on alcohol, eating a healthy, balanced diet, keeping active, staying safe in the sun and others (1), which makes the effective communication of easy to understand healthy lifestyle messages extremely important. Continued action is, therefore, needed to tackle lifestyle-related risk factors for cancer.
The symptoms of cancer can be vague and vary by cancer type, therefore it is paramount people are made aware of symptoms and the importance of screening to ensure people do not go untreated and that the cancer is diagnosed at the earliest opportune moment.
In the UK, lung, bowel, breast and prostate cancers are responsible for:
- 53% of all cancer incidences (2015) (2)
- 45% of deaths from cancer (2016) (3)
In Kirklees between 2010 and 2015 there were approximately 4,500 diagnosed cases of cancer attributable to the top five most common cancers; lung, breast, prostate, colorectal cancer and non-Hodgkin’s lymphoma. If left untreated cancer commonly causes death (4).
What would an asset-based approach to cancer look like?
Health assets are those things that enhance the ability of individuals, communities and populations to maintain and sustain health and wellbeing. These include things like skills, capacity, knowledge, networks and connections, the effectiveness of groups and organisations and local physical and economic resources. They also include services or interventions that are already being provided or beginning to emerge which contribute to improved health and wellbeing outcomes.
Assets are hugely important to how we feel about ourselves, the strength of our social and community connections and how these shape our health and wellbeing. As part of our KJSA development we are piloting a range of methods to capture and understand the assets that are active in Kirklees.
Bowel cancer screening
In 2016 Kirklees Public Health Department used a community engagement approach to increase bowel screening in areas of high risk and low screening adherence. Prior to the start of the Accelerate, Communicate, Evaluate (ACE) project the local community engagement teams carried out baseline awareness, raising engagement in a number of high-risk communities on bowel cancer screening. Many of these areas had high South Asian populations. This work highlighted recurring themes around barriers to bowel screening participation, what worked well in terms of good practice and barriers to awareness raising.
The model involved the engagement team attending a range of establishments such as workplaces, lunch clubs, community events and sport/theatre establishments in the identified high-risk areas. The engagement team promoted bowel cancer awareness information, symptom advice (call to action), lifestyle advice and facilitated the ordering of screening kits at the end of each session, for anyone aged 60 or over who had not completed a kit in the last two years and were not due to receive one in the near future.
A total of 107 kits were ordered for members of the community by the community engagement team.
Kirklees has since begun to pilot a project titled ‘Call for Kit Clinics’. This is a project that was started in Lancashire and was run by the Health Promotion Specialists from the Bowel Cancer Screening Programme (BCSP). The learning and development of this project has been applied in Kirklees to a pilot practice. This project targets people who have previously missed or not completed a bowel screening kit. These patients are contacted and invited to an appointment with a nurse from the BCSP. This appointment involves discussing reasons for not having completed the kit, dispelling any myths and generally supporting the patient to understand the importance of screening. If the patient is in agreement, a bowel screening kit is ordered for them. The initial evaluation of the first pilot demonstrated very positive results and it is hoped the project will now be rolled out to practices which have a low uptake of bowel screening.
Cervical screening
Kirklees Public Health is also working on a cervical screening project which aims to increase participation in cervical screening, particularly in the younger cohort (25-29 year olds) within North Kirklees. NHS England are identifying GP clusters in Kirklees which have a low uptake of cervical screening. Kirklees Public Health are assessing the possibility of setting up a drop-in evening clinic in this area for women who do not feel they can attend their GP practice for various reasons. The clinics will build in some form of evaluation to aid understanding of why women in these areas feel they cannot attend for cervical screening with the view of resolving some of these issues going forward. This work is in the very early stages and there is no confirmation as yet that the project will be feasible.
What are the community assets and actions around cancer?
There are a number of cancer services for people in Kirklees including the NHS, independent sector, local authority, and the voluntary sector, addressing different needs and offering different levels of support for cancer patients and their families.
Asset-based approaches are an integral part of community development. They are concerned with facilitating people and communities to come together to achieve positive change using their own knowledge, skills and lived experience of the issues they encounter in their own lives.
Asset-based community development (ABCD) is a specific framework used to steer processes for community building. It starts by making visible and explicitly valuing the skills, knowledge, connections and potential in a community. Once identified, the process seeks to connect the assets – residents, local organisations and informal community groups – to build strong relationships. The council aims to ensure people are aware of the risks and symptoms associated with cancer through promotion and engagement targeted at high-risk groups. There are also a number of cancer support services across Kirklees, aimed at supporting people and their families post diagnosis (see additional resources at the end of this section).
Macmillan are gathering feedback around the Recovery package at present and what service users want/need after they complete treatment, so this could inform future decisions around patient services and care.
Carers play a vital role in supporting people with cancer. It is estimated that there are almost 1.5 million people in the UK caring for someone with cancer (5). The Carers section of the KJSA has more information about carers and how the needs of carers may be addressed.
What significant factors are affecting this issue?
- Cancer impacts on individuals and their family/friends. People who previously have lived independently may find themselves requiring support following a diagnosis.
- The Lancet, Public Health suggests associations exist between factors indicative of the extent of social connectivity in older people (aged 53–69 years) and their attendance (or not) at routine screening and other preventive health services, indicating that social isolation is a barrier to screening (6).
- Emotional and financial strain due to the impact of cancer can also become problematic for people and support services can be in high demand or be limited.

- In Kirklees in 2016, 54.8% of adults were achieving at least 150 minutes of physical activity a week (7), meaning just under half of the adult population in Kirklees were not achieving this, adding to the risk of obesity and ill health.
Smoking is associated with an increased risk of cancer in general and it is strongly correlated with lung cancer. Smoking is responsible for 85% of all cases of lung cancer (1). People who quit smoking can reduce their risk of developing lung cancer significantly.
The 2016 CLiK survey (7) reported levels of smoking had fallen significantly since 2012. One in eight Kirklees residents now uses e-cigarettes, with the biggest motivator being that it is a ‘healthier alternative’ (44% of e-cigarette users) and that it is ‘cheaper than smoking’ (34% of e-cigarette users). 78% of those who do smoke cigarettes would like to stop.

Some people inherit damaged DNA from their parents, which can give them an increased risk of certain cancers.
Certain medical conditions or immune system problems, and some medicines or treatments, may be linked to an increased risk of some types of cancer. These factors are not included under the preventable cancer factors, because most are not avoidable (1).
The most common cancers are largely preventable; however, prostate cancer is a notable exception, because it is not clearly linked to any preventable risk factors.
Research shows approximately 42% of cancer cases each year in the UK are linked to a combination of 14 major lifestyle and other factors. The proportion is higher in men (45%) than women (40%), largely due to sex differences in smoking (1).
The ‘Which groups are affected most by this issue?’ section give further details on age, deprivation and ethnicity and how these can affect cancer risk.
Awareness
The standardised incidence rate for lung cancer in Kirklees is significantly worse than the England average.
Mortality due to lung cancer in Kirklees is significantly higher than other cancer types. This is most likely due to the fact there is no screening programme available for lung cancer and, therefore, early diagnosis is less likely and a large number of people present late. The numbers of cancer deaths by cancer type between 2010 and 2015 show that lung cancer is an outlier, claiming almost three times as many lives as the next biggest killer (colorectal cancer).
Data source:(4)
People can be diagnosed with cancer through a variety of routes: screening, GP referral and emergency presentation. Emergency presentation routes suggest people need to be more aware of the signs and symptoms of cancer, in order to support earlier diagnosis, thus avoiding emergency presentation routes which lead to later diagnosis and worse outcomes.
The graph below shows how lung cancer in Kirklees is more likely to be diagnosed via two week wait (referral from a GP) or emergency presentation (presenting at A&E). Greater Huddersfield CCG and North Kirklees CCG has a significantly higher rate of emergency presentations for lung cancer than England.
It should be noted that although both CCGs have higher rates of emergency diagnoses for lung cancer, compared to England, this is not reflected in significantly higher late-stage diagnoses.
North Kirklees also has significantly higher percentage of emergency presentations for breast and colorectal cancers than England. In the case of breast cancer, this percentage is also significantly higher than Greater Huddersfield.
Survival data at Kirklees level could only be identified for lung, breast and colorectal cancer, at a single year post-diagnosis. This may be too short a time frame for differences between England and Kirklees to become evident. There is no statistical difference between England and Kirklees for any of the three cancers.
What does the local data tell us?
National screening programmes operate for breast, colorectal and cervical cancer. Screening programs have the effect of potentially increasing incidence in the short term, as they identify new cases, but should bring longer-term benefits through earlier diagnosis and reduced mortality.
The chart below presents the number of diagnosed cases of cancer in Kirklees over the six year period 2010 to 2015, for the top five most common cancers; lung, breast, prostate, colorectal cancer and non-Hodgkin’s lymphoma. In addition liver cancer figures have been provided. Cervical cancer figures have been suppressed due to lower numbers and, therefore, there are no figures available.
Data source: (4)
Further data for breast and colorectal cancer are presented at CCG level in the chart below.
Breast Screening
Attendance for breast cancer screening in Kirklees is on a downward trend. In Kirklees, 76.3% of women were screened in 2013 compared to 75.9% in 2014. In 2015, Healthwatch reported one quarter (24.1%) of women in Kirklees aged 50-70 who are eligible for breast screening for cancer were not taking up their invitation (8). There is also a low awareness amongst women of symptoms. Approximately 30% of all women in England diagnosed with breast cancer report a symptom other than a lump. However, research by Healthwatch shows that when asked to name symptoms of breast cancer, only half of women over 70 (48%) could name a symptom aside from a lump (8).
Some of the signs and symptoms of breast cancer can include:
- a lump in the breast
- a change in the size or shape of the breast
- dimpling of the skin or thickening in the breast tissue
- a nipple that’s turned in (inverted)
- a rash (like eczema) on the nipple
- discharge from the nipple
- swelling or a lump in the armpit
- pain or discomfort in the breast that doesn’t go away.
The previous chart shows the incidence and mortality figures for North Kirklees and Greater Huddersfield between 2012 and 2016.
Standardised mortality rates allow for comparisons across regions. In the chart below, the age-standardised mortality rates for the two Kirklees CCGs can be compared against the England rate.
Which groups are most affected by this issue?
Age
Cancer incidence increases with age. The graph below shows that on average each year 50% of cancer cases were in people aged 70 and over; this is usually due to DNA damage over time. There are also more cases in males than females.
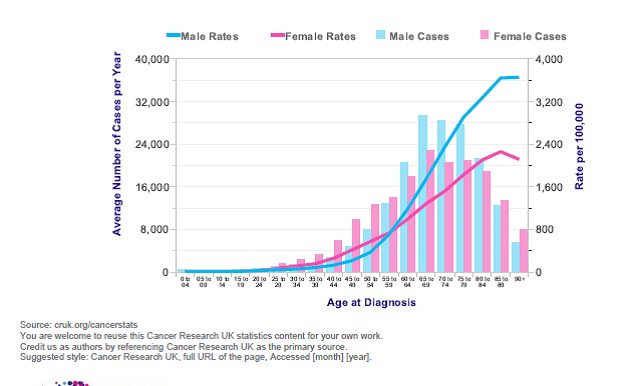
Image source: Cancer Research UK (cruk.org/cancerstats)
Young people with cancer
Although cancer is more common in older people, it can affect younger people. Key national findings from Public Health England’s National Cancer Registration and Analysis Service (NCRAS, 2001-2015) include:
- Mortality rates of all cancers combined in 13 to 24 year olds have decreased from 42.9 per million in 2001 to 32.3 per million in 2015.
- The largest reduction in mortality by diagnostic group in England between 2001 and 2015 has been in Leukaemias. There were also reductions seen in mortality from Central Nervous System tumours, bone cancer and in lymphoma.
- Five-year survival rates for cancer in 13 to 24 year olds have risen from 83% females and 80% males in (2001-05) to 87% females and 84% males (2007-11).
- There are statistically significant variations in incidence and survival rates of cancer in 13 to 24 year olds based on geography and deprivation.
- The incidence of cancer in 13 to 24 years olds in England has increased from a crude rate of 233.1 per million in 2001, to 299.7 per million in 2015.
The main types of childhood cancer are shown below:
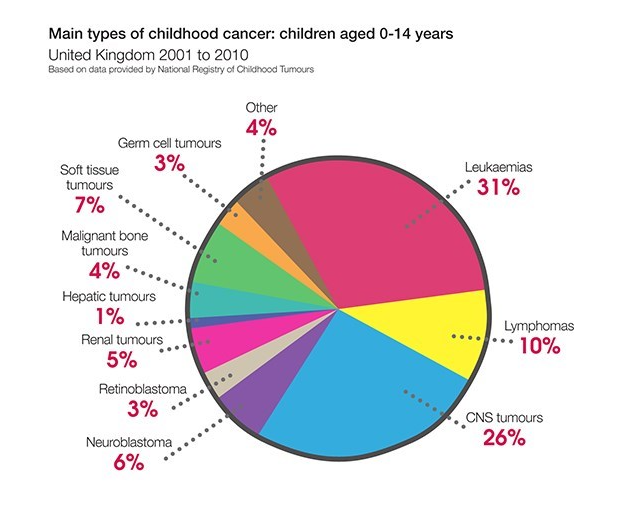
Image from Children with Cancer UK web site (www.childrenwithcancer.org.uk)
There is some evidence that breastfeeding lowers the risk of leukaemia in children, with studies showing breastfeeding for 6 months or longer was associated with a 19% lower risk for childhood leukaemia and with other studies showing that those ‘ever breastfed’ compared with ‘never breastfed’ were associated with an 11% lower risk for childhood leukaemia (9).
The causal factors contributing to childhood cancer are unclear. According to the Children with Cancer UK web site: “Despite a wealth of research, much uncertainty remains over what causes cancer in children… Research is complicated by the fact that there are many different factors which may cause cancer in children. Exposure to more than one of these factors is probably necessary – and probably at different stages of a child’s life.”
Sex
More cancers were registered in males (153,061) than females (146,862). Across the majority of cancer sites more males are diagnosed with cancer than females.
The graph below illustrates that males have a higher incidence of cancer in most sites than females. Breast and prostate cancer account for the highest incidences of cancer.
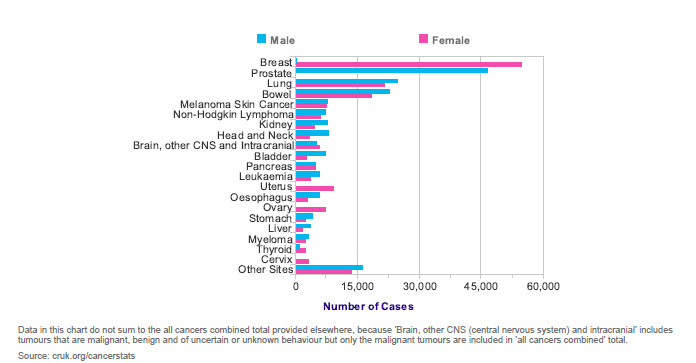
Image source: Cancer Research UK (cruk.org/cancerstats)
Obesity
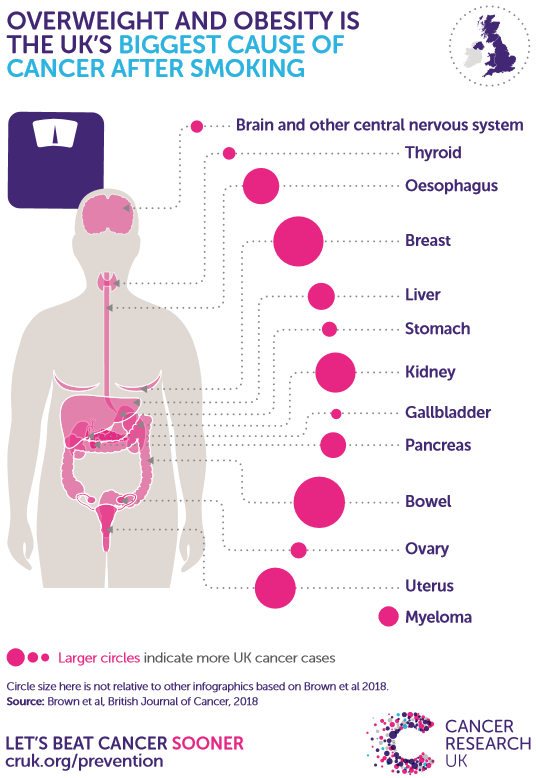
Image source: Cancer Research UK (10)
Overweight and obesity is associated with increased risk of several cancers, including uterine, kidney, esophageal, gallbladder, bowel, pancreas and breast cancers.
Incidence of some overweight- and obesity-related cancers including uterine, kidney and bowel cancer is increasing, at least partly due to increasing prevalence of overweight and obesity. Cancer incidence is expected to rise further if current trends in overweight and obesity prevalence persist (10).
Ethnicity
In Kirklees in 2011 the black and minority ethnic (BME) population group accounted for 88,188 of the population in Kirklees (11). Within the population of Kirklees there were 10,775 people who could not speak English well or at all. This may have had a direct impact on screening statistics due to lack of awareness/understanding.
Overall the incidence of cancer in the BME population in England is lower than that in the white population. However, this varies for different BME groups and cancer types (12):
- Asian, Black, Chinese and Mixed ethnic groups have significantly lower risk of getting any of the four major cancers (breast, prostate, lung and colorectal) compared to White people. Males and females in the Asian, Chinese and Mixed ethnic groups are between 20% and 60% less likely to get cancer than those from the White group.
- Black females are between 10% and 40% less likely to get cancer than White females; in contrast, there is no evidence that Black males have differing risks compared with White males.
- Black males are up to three times more likely to get prostate cancer than White males.
- Black people are nearly twice as likely as White people to get stomach cancer.
- Asian people are up to three times more likely to get liver cancer than the White population.
- Black and Asian females aged 65 years and over are at higher risk of cervical cancer compared with White females.
Deprivation
Kirklees is the 101st most deprived local authority in England (out of 326) based on the Index of Multiple Deprivation 2015 (rank of average ranks method), which is an improvement of 6 places since 2010 (13).
Kirklees has significantly larger proportion of older people who are living in deprivation than the England average and significantly more people than the England average living in income deprivation (14).
Evidence shows that people in deprivation are less likely to complete bowel screening than those of a more affluent position.
Uptake in the England for all the cancer screening programmes shows a gradient by socioeconomic status (15, 16).
Learning Disabilities
People with a learning disability demonstrate a lower uptake in screening programmes (17) and, therefore, they are a target group for Kirklees, with the aim of increasing screening participation in this group. Kirklees Public Health are working closely with Greater Huddersfield CCG and Cloverleaf Advocacy amongst other organisations to work on a project aimed at making screening and health services more accessible to people with a learning disability.
Where is this causing greatest concern?
Cancer can add pressure to emergency services and the local health economy (including local A&E departments). It is, therefore, important for the council and other organisations to reduce risk in the population and to encourage early diagnosis to prevent emergency presentations, which lead to worsening outcomes for the population and the healthcare system.
In Kirklees there are differences between North Kirklees and Greater Huddersfield. The maps below shows areas of concern (shaded a darker green) for breast, bowel and lung cancer incidence in Kirklees.
Lung cancer Incidence – Kirklees
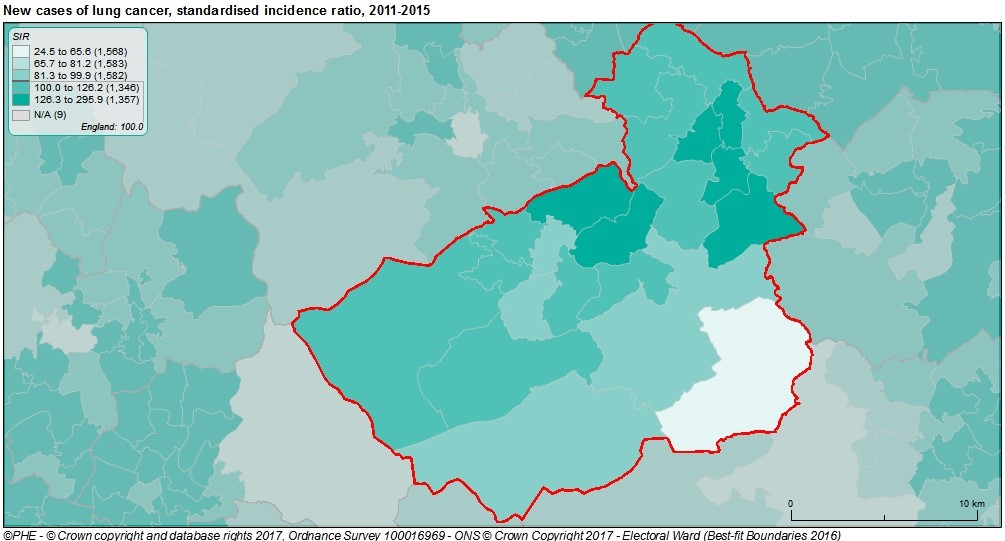
Image from Local Health web site (14)
The graph above shows the lung cancer standardised incidence rates for Kirklees, with Heckmondwike, Batley West, Dewsbury West, Dewsbury South, Dalton and Ashbrow showing the highest incidence.
Breast cancer incidence – Kirklees
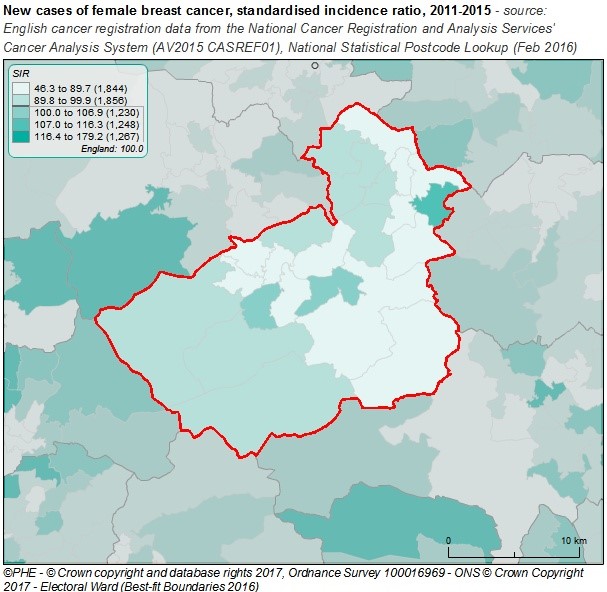
Image from Local Health web site (14)
The data above shows the standard incidence rates for breast cancer in Kirklees, with Dewsbury East, Crosland Moor and Netherton and Almondbury having the highest incidence within Kirklees.
Colorectal cancer incidence – Kirklees
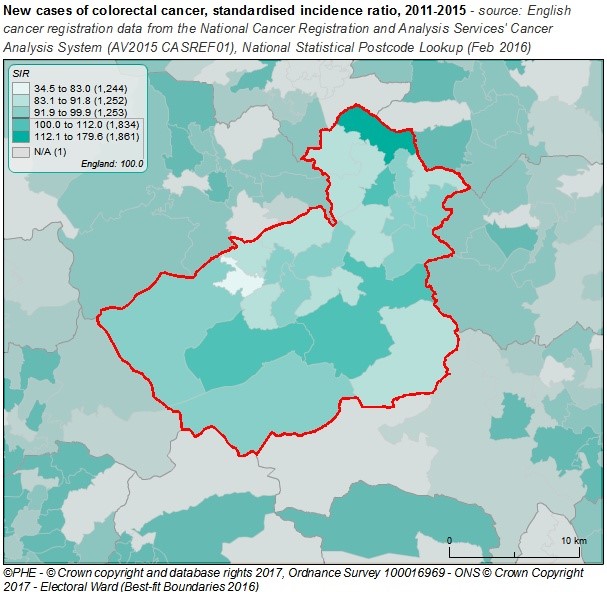
Image from Local Health web site (14)
The above graph shows the standardised incidence rates for colorectal cancer in Kirklees, with Holme valley North, Kirkburton, Heckmondwike and Birstall and Birkenshaw showing the highest incidence.
Views of local people
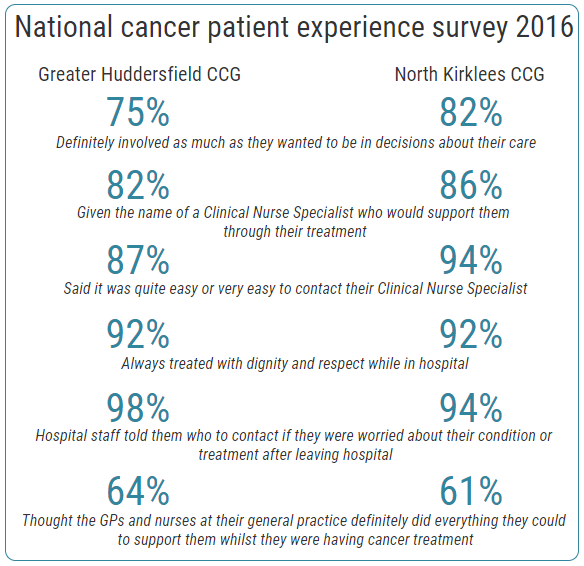
The National Cancer Patient Experience Survey published in July 2017 asked people with cancer their views on their care. The survey had over 72,000 respondents. When asked to rate their care on a scale of zero (very poor) to 10 (very good), respondents gave an average rating of 87.4% (favourable), a statistically significant increase on the previous year’s score.
Key findings of the national cancer patient experience survey 2016 for both Kirklees CCGs are shown below (18):
What could commissioners and service planners consider?
Findings from a questionnaire produced by Kirklees Public Health, Locala and NHS England which targeted parents who had refused their child having the HPV vaccine showed evidence of misunderstanding of the vaccine and its purpose.
Commissioners and service planners could consider the following:
- Myth busting – addressing the misconceptions around the HPV vaccine.
- Local leaflets addressing the myths and concerns locally.
- The HPV vaccine has now been approved for boys, promotion around this will need to commence in Kirklees.
- Cervical screening participation is lower in the 25-39 age group than the 40-64 age group. Work to improve participation in the younger cohort needs to take this into consideration when planning and designing projects.
- A ‘drop in’ cervical screening clinic which will target areas in Kirklees which have low uptake of cervical screening, including low-uptake groups (25-29 year olds, Muslim women and people with a learning disability).
- ‘Call for Kit Clinic’ roll out in low uptake practices across Kirklees. A bid has been submitted to help fund this work.
- Lung cancer opportunistic screening in various locations across Kirklees.
- Raising awareness of lifestyle issues in relation to cancer – making these links clear and promoting ways to improve lifestyle and reduce cancer risk.
- Ensuring breast screening is accessible to all women, addressing potential cultural and religious issues.
- Promote cancer messages via a variety of channels, to be inclusive of the hard-to-reach population. Working with local community groups to support this work.
- Ensure screening is accessible to people with a learning disability, working with service users to understand needs and addressing these needs by putting solutions in place to increase attendance for this group. Promotional materials, letters and other forms of communication need to be in an easy-read format.
- In relation to the connection between people who are socially disconnected and screening behaviour, processes could be implemented to identify older people who are already at risk of becoming socially disconnected and, therefore, vulnerable. The Lancet, Public Health suggests an approach could be incorporated within mandated primary-care checks, or triggered by a response to register important life events such as widowhood. A coordinated approach across health care, social care, and the community is required.
- Promote the use of the Kirklees online platform ‘My Health Tools’ (www.myhealthtools.uk) to help people living with long term health conditions to find information, resources and support.
References and additional resources/links
- CRUK (2016). Causes of cancer. CRUK, UK. http://www.cancerresearchuk.org/about-cancer/causes-of-cancer
- Cancer Research UK web site, Cancer incidence statistics
https://www.cancerresearchuk.org/health-professional/cancer-statistics/incidence - Cancer Research UK web site, Cancer mortality statistics
https://www.cancerresearchuk.org/health-professional/cancer-statistics/mortality - Public Health England. Cancer Services web site: https://fingertips.phe.org.uk/profile/cancerservices
- MacMillan Cancer Support web site: https://www.macmillan.org.uk/information-and-support/organising/practical-preparation-for-treatment/looking-after-someone/being-a-carer.html
- Stafford, M., von Wagner, C., Perman, S., Taylor, J., Kuh, D., & Sheringham, J. (2018). Social connectedness and engagement in preventive health services: an analysis of data from a prospective cohort study. The Lancet Public Health, 3(9), e438–e446. Available here: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6123501/
- Kirklees Council, NHS Greater Huddersfield CCG, & NHS North Kirklees CCG. (2016). Current Living in Kirklees Survey.
- Healthwatch (2015) women not attending breast screening. Healthwatch, UK. https://healthwatchkirklees.co.uk/news/one-quarter-of-women-in-kirklees-not-attending-breast-screening/
- Amitay, E. L., & Keinan-Boker, L. (2015). Breastfeeding and Childhood Leukemia Incidence A Meta-analysis and Systematic Review. JAMA Pediatr. 2015;169(6):e151025. doi:10.1001/jamapediatrics.2015.1025, 169(6). Retrieved from https://jamanetwork.com/journals/jamapediatrics/fullarticle/2299705
- CRUK (2015) Overweight and Obesity, CRUK, UK. http://www.cancerresearchuk.org/health-professional/cancer-statistics/risk/overweight-and-obesity#heading-Zero
- ONS (2011) National Census data
- NCIN (2009) Cancer Incidence and Survival by Major ethnic group, NCIN http://www.ncin.org.uk/view.aspx?rid=75
- Shackelton, A. (2015). The Index of Deprivation 2015: Kirklees Report. Retrieved from Index of Multiple Deprivation 2000 (IMD2000) (kirklees.gov.uk)
- Local Health web site, Public Health England (www.localhealth.org.uk)
- Maheswaran, R., Pearson, T., Jordan, H. and Black, D. (2006). Socioeconomic deprivation, travel distance, location of service, and uptake of breast cancer screening in North Derbyshire. Journal of Epidemiological Community Health [Online], 60. 208 -212.
- Bang, J.Y., Yadegarfar, G., Soljak, M. and Majeed, A. (2012). Primary Care factors associated with cervical screening coverage in England. Journal of Public Health [Online], 34, 532-538.
- Connolly, J. (2013). Barriers to access to cancer screening for people with learning disabilities: a review. The Lancet, 382(S29). Retrieved from https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(13)62454-X/fulltext
- Quality Health. (2017). National Cancer Patient Experience Survey. Retrieved December 14, 2018, from http://www.ncpes.co.uk/reports/2016-reports/local-reports-1/clinical-commissioning-groups
Additional resources
This list is correct as of February 2019, but may go out of date. Please contact the organisation first before making travel arrangements.
Rosewood palliative care day therapy (Dewsbury hospital) for patients with incurable cancer. Address: Rosewood Centre, Dewsbury District Hospital, Halifax Road, Dewsbury WF13 4HS
Telephone: 01924 512039
Drop in Macmillan cancer support
Every Thursday 10-12 at the Cavell unit (Dewsbury hospital) for patients who require information and support
The Jayne Garforth Cancer Information Centre
Huddersfield Royal Infirmary
Monday to Friday 9.00 – 16.00.
The centre is not always manned by the Manager throughout this time. If you would like an appointment with the service manager please telephone 01484 343614 or 07554415564. Alternatively you can email the service on cancerinformationservice@cht.nhs.uk
Headstrong (Hair Loss Service)
For more information on this service please contact the Macmillan unit in Huddersfield Royal Infirmary on: Greenlea Unit HRI: 01484 343614
Kirkwood Hospice
Address: Kirkwood Hospice, 21 Albany Road, Dalton, Huddersfield, West Yorkshire HD5 9UY.
Telephone: Reception: 01484 557900
Cancer Research UK
https://www.cancerresearchuk.org/
Macmillan Cancer Support
Website: https://www.macmillan.org.uk/
Find local support: https://www.macmillan.org.uk/in-your-area/choose-location.html
Telephone: The Macmillan Support Line can help with clinical, practical and financial information. Please call us on 0808 808 00 00 (Monday-Friday, 9am-8pm).
Breast Cancer support group
This group meets on the first Monday of the month from 10 am – 11.30 am at The Keys Restaurant, St Peter’s Church, Huddersfield.
Breastfriends (Halifax and Huddersfield)
Briar Court Hotel, Halifax Road, Birchencliffe, Huddersfield, HD3 3NT.
First Thursday of the month at 7.30pm
Calderdale & Huddersfield Bladder Cancer Support Group
Address: Briar Court Hotel, Halifax Road, Birchencliffe, Huddersfield, HD3 3NT.
Telephone: 01484 355269
Briar Court every three months
Be Be Cancer Support
Last Friday of the month. Drop in advice / chat / information.
Group supports everybody.
Befriending, Bereavement support, Cancer information materials, Complementary therapies, Counselling, Information, Internet use available and Support from Health Professionals. Please contact the group for further details.
Lorraine Newton on 01924-400093 (Mon-Sun) or email: info@bebebeauty.co.uk
Mid Yorkshire Warblers Head and Neck cancer group
Head & neck cancers
Services provided include: Carers, Relatives, Young adults affected by cancer, Head and Neck, Home visiting, Bereavement Support, Befriending, Cancer information materials, Support from Health Professionals 10am to 12pm third Friday of the month, Pinderfields Hospital
Just come along to the next meeting, or get in touch with us on the details below.
Helen Chadwick or Nina Corfield on 01924 542250 /01924 542544 (Mon-Fri, 8am-4pm); Email: helen.chadwick2@midyorks.nhs.uk
My Health Tools: www.myhealthtools.uk
Date this section was last reviewed
22/02/19 (JH)
