
 Infectious disease
Infectious disease
Headlines
Why is this issue important?
Modern public health system, vaccines and antibiotics have revolutionised the way we protect ourselves from infections. However, infectious disease still poses a problem for Kirklees residents, as it does nationally and internationally.
Infections due to antibiotic-resistant bacteria are threatening modern health care. Estimating their incidence, complications, and attributable mortality is challenging and has triggered the need to develop coordinated and comprehensive national, European, and global action plans. There is a need in Kirklees as well as nationally for ongoing work to reduce the volumes of antibiotics that are used inappropriately, to try and reduce antimicrobial resistance.
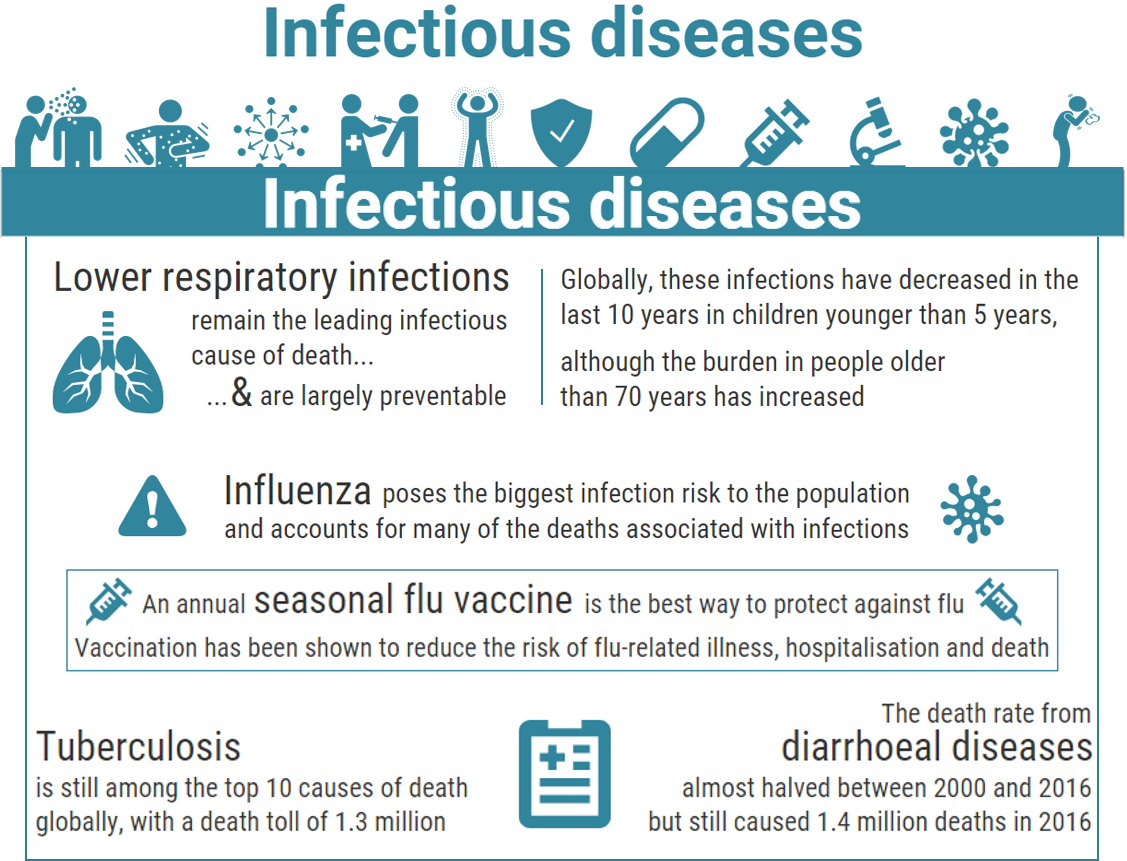
Lower respiratory infections remain the most deadly communicable disease, causing 3.0 million deaths worldwide in 2016. The death rate from diarrhoeal diseases almost halved between 2000 and 2016, but still caused 1.4 million deaths in 2016. Similarly, tuberculosis killed fewer people during the same period, but is still among the top 10 causes with a death toll of 1.3 million (1). Infectious diseases such as tuberculosis (TB) remain an issues in Kirklees. Despite reductions in incidence Kirklees has a higher incidence rate than nationally and the continued work towards the goals of the TB strategy remain important (2).
Influenza poses the biggest infection risk to the population and accounts for many of the deaths associated with infections. The elderly and those with long term conditions are particularly vulnerable to the flu virus. Kirklees uptake in influenza vaccine (along with the national uptake) could be improved, thus preventing these complications in the vulnerable (2).
HIV/AIDS is no longer among the world’s top 10 causes of death, having killed 1.0 million people in 2016 compared with 1.5 million in 2000 (1). HIV is covered in more detail in the Sexual health section of the KJSA.
What are the community assets and actions around this issue?
Infectious diseases are caused by organisms — such as bacteria, viruses, fungi or parasites. Many organisms live in and on our bodies. They’re normally harmless or even helpful, but under certain conditions, some organisms may cause disease/infections.
Some infectious diseases can be passed from person to person. Some are transmitted by bites from insects or animals. And others are acquired by ingesting contaminated food or water or being exposed to organisms in the environment.
Immunisation remains one of the most important, and cost-effective, health interventions. Some life-saving vaccines cost just pennies, require only one dose, and provide immunisation throughout life. Immunisation programmes play an important role in the prevention of epidemics: through immunisation of specific disease and with wider health protection. Vaccination greatly reduces the burden of infectious diseases and has resulted in dramatic falls in rates of many vaccine preventable diseases in the UK such as polio and measles. Vaccines save lives, prevent disability and help people with serious and long term conditions to stay healthy.
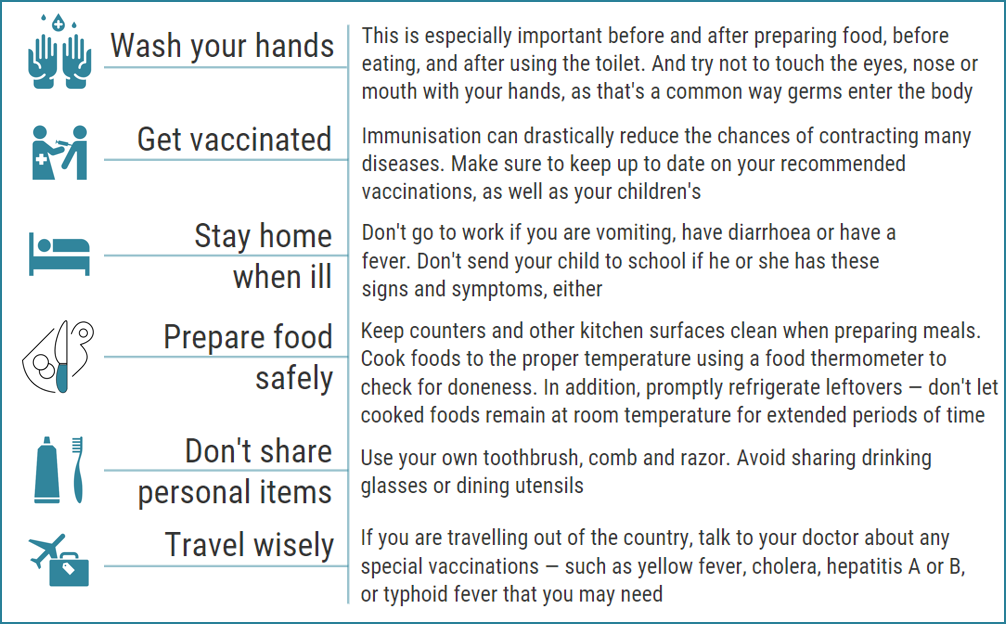
There are other ways you can decrease the chances of getting an infection or passing one on.
Antibiotic resistance
It’s everyone’s responsibility to use antibiotics responsibly. They are not effective against viral infections, including colds and flu. Antibiotic overuse is a serious problem and potentially a threat to everyone’s health. You should be guided by your GP or pharmacist as to whether or not you need an antibiotic.
Antibiotic resistance is a threat to human health and to medicines worldwide. Overuse and misuse of antibiotics could mean that in the future even the simplest infections cannot be treated and the most straightforward operations cannot be done.
This is an issue that affects every single one of us and could have devastating consequences. It is vital that we tackle this problem urgently so we can safeguard the health of ourselves, our children, and future generations.
Antibiotics should only be used for serious bacterial infections.
Some of the easy ways to help:
- Practice good hand hygiene to help prevent the spread of infection in the first place – wash your hands after using the bathroom, before preparing or eating food, after coughing or sneezing, or if your hands are visibly dirty
- If you don’t need antibiotics, for instance for viral infections, like a cold or flu, don’t take them
- Speak to your GP or pharmacist before you ask for an antibiotic – don’t demand antibiotics from your GP, they will make the decision on whether you need them or not
- If you’re prescribed antibiotics, finish the course or medication (even if you start to feel better)
- Never share antibiotics with anyone else
Factors affecting this issue, groups most affected, and what the local data tells us
Childhood immunisation
Measles
Measles is one of the most highly infectious communicable diseases. It is transmitted by droplet infection. Almost all who are infected develop symptoms. Spending 15 minutes or more in direct contact with someone infected with measles is considered a significant exposure. Measles is spread through coughing, sneezing, close personal contact or direct contact with infected nasal or throat secretions. Immunocompromised patients, pregnant women and unvaccinated infants are at increased risk of severe disease. Measles can lead to serious complications, including blindness and even death. The vaccine is routinely given at 1 year of age, with a second dose at around 3 years and 5 months, as part of the NHS Childhood Immunisation Programme.
The UK achieved WHO measles elimination status last year, so the overall risk of measles to the UK population is low.
Public Health England continues to see imported measles cases in the UK and limited onward spread can occur in communities with low vaccine coverage and in age groups with very close mixing. Almost all recent cases have been in children who were unvaccinated.
MMR vaccination coverage in Kirklees is better than the England average. In Kirklees the percentage of eligible children who received two doses of MMR on or after their first birthday, and at any time up to their fifth birthday was 93.8%, which is higher than the England average of 87.2% (2).
Low vaccine cover leads to higher risk for populations particularly in respect of Measles. As a result of the persisting risk linked to poor vaccine coverage, MMR vaccination still remains a priority in the Kirklees area.
Mumps
Mumps is a relatively mild short term viral infection of the salivary glands that usually occurs during childhood, but can appear in teenagers and young adults. Transmission is by direct contact with saliva or droplets from the saliva of an infected person. Early symptoms include a headache and fever characterised by swelling of the parotid glands which may be one or two sided.
Local further education colleges and universities are often the places outbreaks occur in. Mumps can lead to viral meningitis. Other complications include swelling of the testicles in males and the ovaries in females who have gone through puberty. Other symptoms include pancreatitis, neuritis, arthritis, mastitis, nephritis, thyroiditis and pericarditis. Mumps is rarely fatal but complications include swelling of the ovaries (oophoritis), swelling of the testes (orchitis), aseptic meningitis and deafness. Mumps is a notifiable disease in England and Wales. Not all notified cases are laboratory confirmed. For vaccine uptake, note mumps is part of the MMR vaccine.
Increasing uptake of MMR vaccination with the mumps constituent will increase protection for the population so, as noted, measures are being taken to encourage increased uptake.
Pertussis
Whooping cough (medically known as pertussis) is a serious infection that causes long bouts of coughing and choking, making it hard to breathe. The “whoop” is caused by gasping for breath after each bout of coughing, though babies don’t always make this noise.
Whooping cough is a highly infectious, serious illness that can lead to pneumonia and brain damage, particularly in young babies. Most babies with whooping cough will need hospital treatment, and when whooping cough is very severe they may die.
Research from the vaccination programme in England shows that vaccinating pregnant women against whooping cough has been highly effective in protecting young babies until they can receive their own vaccinations from two months of age.
In contrast to usual disease patterns, which see cases increasing every three to four years in England, whooping cough cases have fallen in all age groups since 2012. The greatest fall has been in young babies targeted by the pregnancy vaccination programme.
Cases of whooping cough in older age groups are still high compared to pre-2012 levels. The number of cases was particularly high in 2016, in line with the typical three to four-yearly peak in disease rates.
Babies can be infected by people with whooping cough in these older age groups, so it is still important for pregnant women to be vaccinated to protect their babies. Babies will still need to have the pertussis constituent in their own primary immunisations as part of the childhood immunisation programme.
In Kirklees Pertussis vaccination coverage for one year olds in 2017/2018 was 95.4%, which is better than the England average of 93.1%. The Pertussis vaccination coverage for two year old in 2017/2018 was 96.5%, which is again better than the national average of 95.1%. (2)
Meningococcal and pneumococcal disease
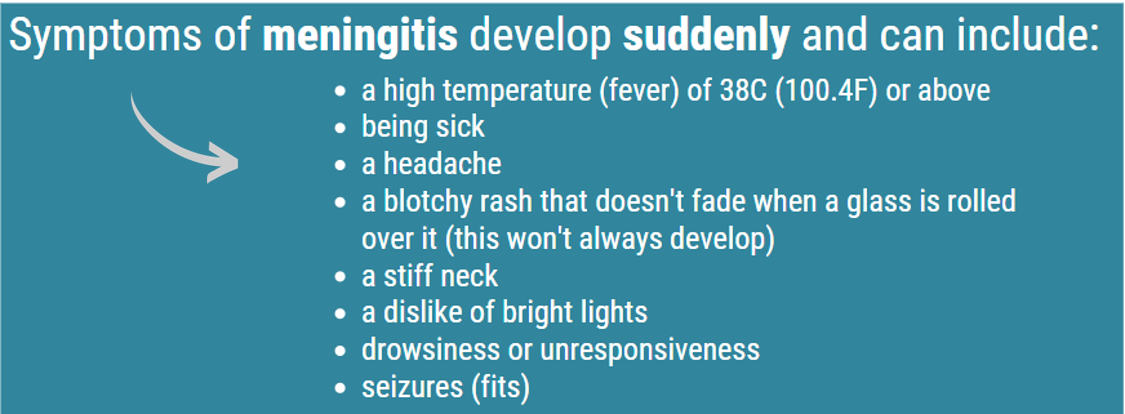
Meningococcal and pneumococcal disease can cause septicaemia and meningitis and can kill. Some survivors of invasive disease have permanent effects including limb amputations, brain damage and hearing loss. The NHS offers vaccination against strains of meningococcus and pneumococcus to specific age groups to prevent invasive meningococcal and invasive pneumococcal disease. Meningitis can affect anyone, but is most common in babies, young children, teenagers and young adults.
Vaccinations against meningitis
A number of vaccinations offer protection against certain causes of meningitis. These include the:
- meningitis B vaccine – offered to babies aged 8 weeks, followed by a second dose at 16 weeks, and a booster at 1 year
- 6-in-1 vaccine – offered to babies at 8, 12 and 16 weeks of age
- pneumococcal vaccine – offered to babies at 8 weeks, 16 weeks and 1 year old
- Hib/MenC vaccine – offered to babies at 1 year of age
- MMR vaccine – offered to babies at 1 year and a second dose at 3 years and 4 months
- meningitis ACWY vaccine – offered to teenagers, sixth formers and “fresher” students going to university for the first time
The UK has the most comprehensive national meningococcal vaccination programme in the world. It aims to protect those most at risk, and the wider population, against meningococcal A, B, C, W and Y disease.
The Joint Committee on Vaccination and Immunisation (JCVI) issued the following statement (3):
Overall cases of meningococcal disease are low across the population primarily because of the excellent vaccine coverage in target groups. Meningococcal disease however, continues to have a devastating impact on individuals and their families. Meningococcal vaccine programme is reviewed more regularly than for most other infections. The JCVI’s latest review noted that the number of meningococcal capsular group C (MenC) cases remain low but there has been a gradual rise over the last few years partly due to a larger increase in cases in the Yorkshire and Humberside region of England. Cases are mainly being seen in infants and older adults.
The aim of the current MenC vaccination programme is to provide direct protection to toddlers, teenagers and young adults and also to provide indirect protection to the wider population by generating herd immunity. Adolescents and young adults are known to be the main carriers of the meningococcal bacteria at the back of their nose and throats. Because of this, our meningococcal ACWY (MenACWY) vaccination programme focusses on this age group. As the MenACWY vaccine protects against carriage, vaccinating a high proportion those eligible in this age group will consequently reduce onward transmission to susceptible children and adults.
Vaccine coverage in younger adolescents with MenACWY through the school-based programme is high. Coverage in those older adolescents and young adults who are eligible for the vaccine is lower, including in those who have not entered higher education. JCVI believes that optimum control of MenC disease can only be achieved if vaccine coverage in older adolescents and young adults is improved.
JCVI therefore believes that GPs should be strongly encouraged and supported to improve coverage in those aged 18 to less than 25 years who are eligible for vaccination. It is anticipated that efforts to urgently improve MenACWY vaccine coverage in this age group will lead to a reduction in cases of MenC and MenW disease across the population.
In response to JCVI’s review, the Department of Health and Social Care, NHS England and Public Health England, supported by the Chief Medical Officer, will work to improve MenACWY vaccine coverage in this age group.
Childhood immunisation – the local picture
Overall annual childhood immunisation uptake rates in Kirklees remain high, with most exceeding the World Health Organisation 95 % target.
By 2 years of age the COVER achieved in 2017/18 for Meningitis B is at 100% (2), first MMR dose is at 94.7% and Diptheria, Tetanus, Polio, Pertussis and Hib is at 96.5% (2). HIB/Men C sits below 95 % at 94.0% (2).
Achievement of target levels by age 5 years remains good but is slightly below the 95% target for the fourth doses of diphtheria, pertussis, tetanus and polio (93.7% in 2016/17) (4), and second dose of MMR (93.8% for 2017/18) (2).
Kirklees has higher uptake levels than Yorkshire and Humber and those for England, indicating a greater uptake in the Kirklees area than both regionally and nationally. The drive to improve rates of vaccine uptake will continue in Kirklees.
MenACWY vaccine uptake for September 2017 to August 2018 (School year 9, 13-14 years old) in Kirklees was 92.3% as part of the schools programme; which compares favourably with the overall England uptake of 86.2% for the same time period (5).
Pneumococcal polysaccharide Vaccine (PPV)
Adult Pneumococcal Polysaccharide Vaccine (PPV) is available on the NHS to all adults over 65 years, as this age cohort are considered at higher risk of serious infections. The PPV protects against bacteria which can lead to pneumonia, septicaemia and meningitis. Over 65 year olds require only one vaccine to protect them for life.
Pneumococcal polysaccharide Vaccine (PPV) – the local picture
Adult PPV 2017/2018 in Greater Huddersfield CCG has an uptake of 72.6% (above the lower national threshold of 65%) with a year-on-year increase from 68.5% since 2013/14. North Kirklees CCG has an uptake of 73.0 %, above the lower national threshold of 65% and again showing a year-on-year increase from 65.1 % in 2013/14 (6).
Shingles
Shingles (herpes zoster virus) is caused by the reactivation of the latent varicella zoster virus. Shingles presents as a painful skin rash, which can cause ongoing pain. Shingles can be fatal in people over 70 years old. The national shingles programme is to lower the incidence and severity of shingles in older people. Recommendations are for it to be routinely offered to people aged 70 years. There is also a catch-up programme being rolled out in those aged 70 -79 years based on cost effectiveness and as this age group is likely to have the greatest benefit. Performance shows that, for 2018/19 June data for 70 year olds and 78 year olds, Kirklees has achieved the national lower threshold of 50% but not yet achieved the national standard target of 60%. Public Health is encouraging pharmacies and GP practices to carry out opportunistic vaccination.
Shingles – the local picture
Uptake for the routine age cohort for 01/09/2017 – 31/08/2018 for Kirklees is 55.1% (2) with the figure for those registered patients aged 78 years at 55.5% (catch up programme) (7). 100% of GP practices in Kirklees took part in the data submission.
Human Papilloma Vaccine (HPV)
The national HPV programme was introduced in September 2008 with all girls in school year 8 in England (aged 12 to 13 years) being offered vaccination against HPV infection. HPV protects against the common types of HPV, which are linked to certain types of cancers, including cervical cancer. The HPV is currently offered to girls aged 12-13 (school year 8) with dose 1, this is then followed within 12 months with dose 2. The programme is due to be rolled out to boys in 2019 following recommendations from the Joint Vaccination and immunisation Committee to the Department of Health. Kirklees Public Health is working with Locala and NHS England to increase uptake of HPV. A task and finish group has been set up and includes forward planning, promotion of the vaccine in preparation for the roll out to boys.
Human Papilloma Vaccine (HPV) – the local picture
Figures for vaccine uptake in Kirklees for girls in school year 8 for 2017/2018 show that uptake for 1st dose (one dose by 31/08/2018) was 89.4% and uptake for the second dose was 85.8%. Overall the total coverage for Local Authorities in England for HPV vaccine was 67.8 – 95.3% (8).
Influenza Vaccine
The influenza vaccine protects against influenza and is routinely given in the NHS to:
- Adults 65 years and over
- People with certain medical conditions (Including children in at-risk groups from 6 months of age)
- Pregnant women
- Children aged 2 and 3
- Children in reception class and school years 1,2,3,4 and 5
The vaccine is available at GPs and pharmacies.
The IPC team promote the Influenza vaccine through attendance at various events, providing the public and frontline staff with information about the vaccine and its importance. Information has been distributed to care homes informing staff where to access free Influenza vaccines and the importance for themselves and those in their care.
Influenza Vaccine – the local picture
Seasonal influenza vaccine uptake in GP patients from 01/09/2017 to 31/01/2018 shows Greater Huddersfield CCG uptake for those aged 65 years and over was 72.9%, meeting the lower national threshold of 70%. For those aged 6 months up to 65 years in Greater Huddersfield, the uptake was 51.7 %, meeting the lower national threshold of 50%. North Kirklees CCG reported a 73.9% uptake for those 65 years and over, again meeting the lower national threshold of 70% and a 51.3 % uptake for those aged 6 months up to 65 years old with clinical risk, again meeting the lower national threshold of 50% for this age cohort (9).
Gastrointestinal Infections
The organisms that cause gastro-intestinal infections include viruses, bacteria and parasites, and the identity of the organism can only be confirmed by laboratory testing of a faecal sample. The symptoms of food poisoning can range from vomiting, to diarrhoea and stomach cramps. Those who are elderly or have a condition that weakens the immune system, such as HIV or cancer, have an increased risk of developing more serious symptoms. Local figures are laboratory reported cases; the actual incidence in the community will be higher than reported as not all cases are reported.
Gastrointestinal Infections – the local picture
Food poisoning remained the most frequently notified gastrointestinal infection in Kirklees in 2017. Outbreaks of food poisoning linked to commercial food premises and other public events have declined in recent years reflecting a positive impact from the proactive work led by Kirklees Environmental Health officers.
Viral gastroenteritis
Norovirus is transmitted by eating contaminated food or water or by contact with contaminated objects. Institutional settings, particularly those with vulnerable people such as care homes, hospitals and schools, continue to be severely affected.
Ongoing education with these settings about infection prevention and control continues to contribute to more effective management of outbreaks.
Hospital admissions for gastroenteritis in infants aged under one year in 2016/2017 was 204.1 per 100,000, similar to the England average (10).
Admissions for infants aged one year for gastroenteritis in 2016/2017 was 142.8 per 100,000 (10). This is a higher number of admissions than the England average of 100.7 per 100,000 (10).
Admissions for infants aged two, three and four years for gastroenteritis in 2016/2017 was 77.4 per 100,000 (10). This is a higher number of admissions for this age cohort than the England average of 53.5 per 100,000 (10).
Tuberculosis (TB)
Early diagnosis and treatment is key to preventing further transmission of TB. Delayed diagnosis of potentially infectious cases within a healthcare settings has considerable impact with regard to exposure to staff and patients.
Tuberculosis – the local picture
There were 177 cases of TB reported in Kirklees between 2015 and 2017, with an incidence rate of 13.6 per 100,000, which is not only a reduction on 2014-16 (16.6 per 100,000), but the lowest rate in the last 16 years of three-year average rates (11). It is encouraging that TB incidence is still declining both locally and nationally, however the rate of reduction has slowed. There remains considerable variation in TB rates across Yorkshire and Humber and the gap between the highest burden local authority and other areas is considerable. This is despite significant progress in incidence reduction in the high burden areas.
The NHS England funded latent TB infection (LTBI) testing and treatment programme has now been in place in Yorkshire and Humber since February 2016, covering the four local authority areas identified as having the highest burden of TB (Sheffield, Leeds, Bradford and Kirklees). Those eligible for screening (aged 16 to 35 years, who have entered the UK from a high incidence country within the last five years) are identified in primary care and subsequently screened by single interferon gamma release assay (IGRA).
TB incidence rates for 2015- 2017 (2):
- Kirklees rate is 13.6 per 100,000 population
- Yorkshire and Humber rate is 7.4 per 100,000 population
- England is at 9.9 per 100,000 population
- Bradford is 17.7 per 100,000 population
Despite improvements in the proportion of cases which are microbiologically confirmed, 25% of pulmonary cases nationally were not confirmed, with 38% of all cases not confirmed (12). Only 63% of pulmonary cases nationally had a smear status recorded (12).
Where is this causing greatest concern?
TB is a priority for the whole of Kirklees, due to rates of 13.6 per 100,000 population.
Views of local people
The Tuberculosis (TB) service provides a high quality, nurse-led TB community management service working alongside Public Health, local Acute Hospital Trusts and Public Health England. A survey is carried out annually to gain service users views on the service and to understand if the service is meeting the needs of the population.
94 responses were received and recorded in the 2018 survey.
- Approximately 91% of respondents thought the service was ‘excellent’.
- Approximately 9% of respondents thought the service was ‘OK’.
- None of the respondents thought the service was ‘not good’.
The main themes that emerged from the comments given show the TB team are considered by their patients to be:
- Welcoming
- Friendly and kind
- Informative
- Helpful
What could commissioners and service planners consider?
Tuberculosis
In January 2015, Public Health England and NHS England jointly launched the Collaborative Tuberculosis Strategy for England 2015-2020 (13). The strategy aims to achieve a year on year decrease in TB incidence, a reduction in health inequalities, and ultimately the elimination of TB as a Public Health problem in England.
Kirklees remains in the four Local Authorities with the highest rates of TB in the Yorkshire and Humber region and as such momentum towards the goals of the Collaborative TB Strategy should be maintained. Kirklees has already rolled out a robust LTBI programme and will further develop and consolidate this going forward.
In line with recommendations, national and regional guidance, Kirklees will:
- continue to improve access to services and ensure early diagnosis
- continue to develop and sustain universal access to high quality diagnostics
- continue to improve treatment and care services
- contribute to the national processes on the reduction of drug-resistant TB
- continue to tackle TB in under-served populations
- sustain and develop the new entrant latent TB screening programme
Three final overarching recommendations that relate to the broader aspects of TB control include:
- TB Control Boards (TBCBs) are encouraged to continue their work providing support to local TB control and overseeing local implementation of the TB strategy’s ten areas for action. Kirklees will continue to support this process utilising the Kirklees TB strategy forum.
- CCGs and local authorities are encouraged to use the PHE TB Fingertips tool (http://fingertips.phe.org.uk/profile/tb-monitoring) to assess their local TB burden to support JSNA development and TB commissioning and monitoring. Kirklees will utilise data to inform policy and decision making in conjunction with the TB Control board and the Kirklees Strategy Group
- TB services are encouraged to submit high quality data to strengthen surveillance to support appropriate public health decision making and commissioning. Kirklees will support the collecting of appropriate data to inform this process.
Crucial work to continue to implement the Collaborative TB Strategy needs to continue to strengthen TB control, achieve the Strategy’s goals of a year-on-year decrease in incidence, a reduction in health inequalities and, ultimately the elimination of TB as a public health problem in England.
References
(1) World Health Organization. (2018). The top 10 causes of death. Retrieved from: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
(2) Public Health England (2018) Health Protection, Public Health England, UK. https://fingertips.phe.org.uk/profile/health-protection
(3) Department of Health and Social Care. (2018). JCVI statement on meningococcal vaccination. Retrieved from https://www.gov.uk/government/publications/meningococcal-vaccination-statement-from-jcvi/jcvi-statement-on-meningococcal-vaccination
(4) Public Health England. (2018). Cover of vaccination evaluated rapidly (COVER) programme: annual data. Retrieved February 20, 2019, from https://www.gov.uk/government/publications/cover-of-vaccination-evaluated-rapidly-cover-programme-annual-data
(5) Public Health England. (2019). Meningococcal ACWY immunisation programme: vaccine coverage estimates. Retrieved February 20, 2019, from https://www.gov.uk/government/publications/meningococcal-acwy-immunisation-programme-vaccine-coverage-estimates
(6) Public Health England. (2018). Pneumococcal polysaccharide vaccine (PPV): vaccine coverage estimates. Retrieved February 20, 2019, from https://www.gov.uk/government/publications/pneumococcal-polysaccharide-vaccine-ppv-vaccine-coverage-estimates
(7) Public Health England. (2018). Herpes zoster (shingles) immunisation programme 2017 to 2018: evaluation report. Retrieved February 20, 2019, from https://www.gov.uk/government/publications/herpes-zoster-shingles-immunisation-programme-2017-to-2018-evaluation-report
(8) Public Health England. (2018). HPV vaccine coverage annual report for 2017 to 2018. Retrieved February 20, 2019, from https://www.gov.uk/government/statistics/hpv-vaccine-coverage-annual-report-for-2017-to-2018
(9) Public Health England. (2018). Seasonal influenza vaccine uptake amongst GP Patients in England. Retrieved from https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/684554/Seasonal_flu_vaccine_uptake_GP_patients_2017_2018_01_September_31_January_CCG_AT.pdf
(10) Public Health England. (2019). Child and Maternal Health Profile. Retrieved February 20, 2019, from https://fingertips.phe.org.uk/child-health-profiles#page/0/gid/1938133226/pat/6/par/E12000003/ati/102/are/E08000034
(11) Public Health England. (2019). Public Health Outcomes Framework. Retrieved February 20, 2019, from http://www.phoutcomes.info/
(12) Public Health England. (2018). Tuberculosis in England: 2018 Presenting data to end of 2017. Retrieved from https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/774091/TB_Annual_Report_2018_2.pdf
(13) Public Health England. (2015). Collaborative tuberculosis strategy for England. Available here: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/403231/Collaborative_TB_Strategy_for_England_2015_2020_.pdf
Date this section was last reviewed
20/02/19 (JH)
