
 Chronic kidney disease
Chronic kidney disease
Headlines
Why is this issue important?
The kidneys regulate the body’s fluid levels, filter waste and toxins from the blood, release hormones to regulate blood pressure, stimulate the production of red blood cells, and help control how the body uses vitamins and minerals to build things like healthy bones.

Decreased functionality of the kidneys is known as chronic kidney disease (CKD). Unlike diseases of other organs such as the heart and lungs, it is difficult to tell if you have CKD without simple and freely available tests. It is only as the disease progresses and starts to causes irreversible damage that symptoms may start to appear (2). These might include weight loss, poor appetite, swollen ankles, tiredness, shortness of breath, and blood in the urine, frothy urine, an increased need to pass urine, difficulty sleeping, itchy skin, muscle cramps, feeling sick, headaches, and erectile dysfunction.
The NHS Choices web site has a well explained definition of CKD, including sections on symptoms, diagnosis, treatment and prevention. The NHS Choices explanation avoids technical terms, however for those more familiar with the topic, the below paragraph summarises some of the management options around CKD, to emphasise the importance of prevention.
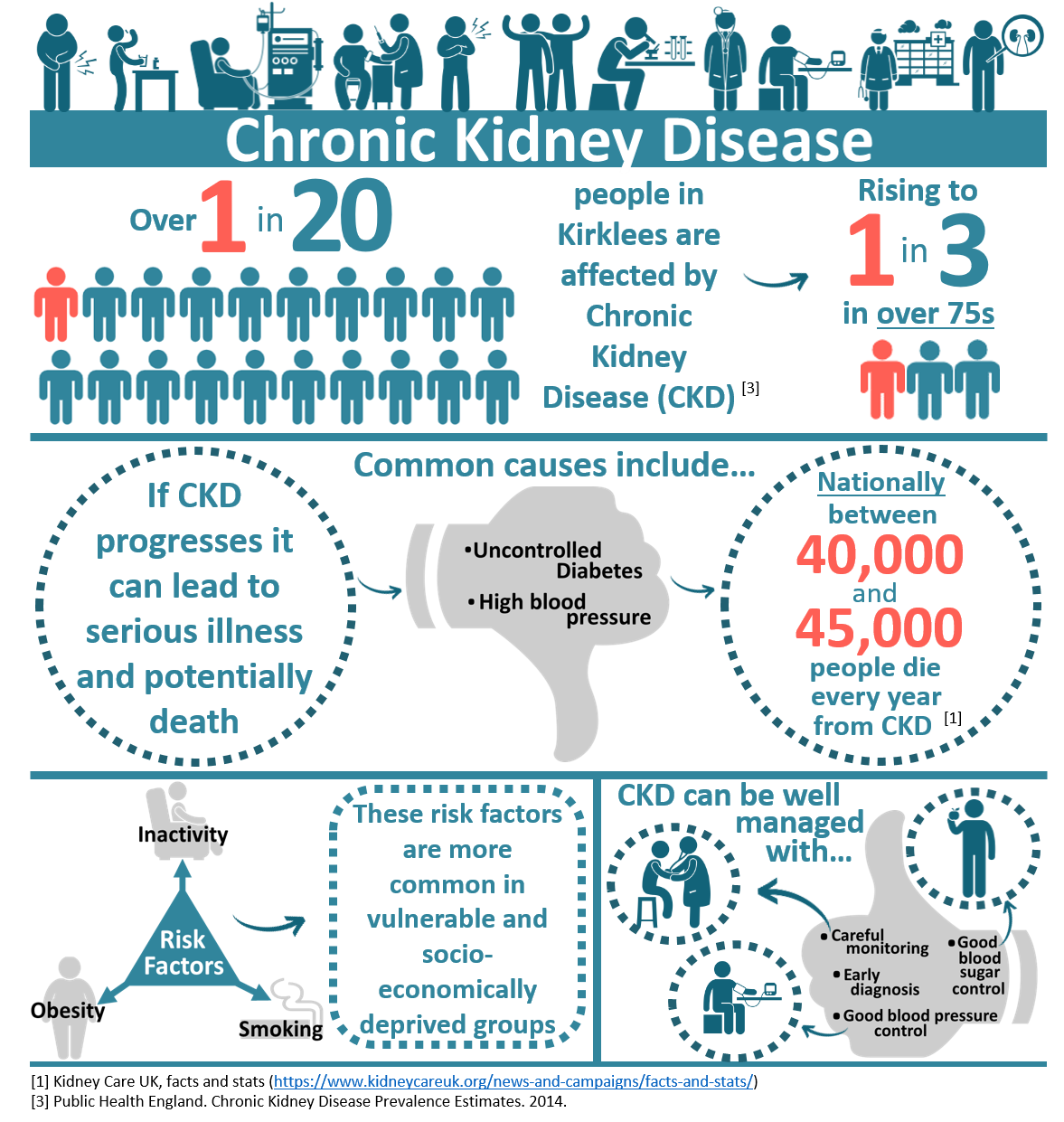
CKD is initially managed through lifestyle changes and medications to control associated problems such as high blood pressure and anaemia (2). With good control of blood pressure and blood sugar levels (in diabetes) it may be possible to stop CKD from becoming more advanced. If CKD progresses it can cause end stage renal failure (ESRF), where the kidneys are no longer able to carry out their role in the body. In ESRF unregulated fluids, minerals, and toxins build up in the blood, without management this would cause people to feel ill, and eventually could lead to death. ESRF can be managed symptomatically, with renal replacement therapy (RRT) or with a kidney transplant. RRT for ESRF involves artificial replication of the kidney’s functions, through peritoneal dialysis or haemodialysis. Treatment with RRT and transplant is not suitable for everyone: the interventions are risky; have side effects; significant lifestyle implications; and neither reverse the damage already done elsewhere in the body. Prevention and early detection are therefore of paramount importance in managing CKD.
Community assets and action
What would an asset-based approach to CKD look like?
So far the focus has been on the problems caused by CKD, however when considering these, it is important to also consider what potential solutions are already in place in Kirklees, and how we could make best use of them.

The KJSA sections listed in the next paragraph below are important to build in to approaches in managing CKD.
What are the community assets and action around this?
CKD is predominantly caused by diabetes and hypertension (high blood pressure). The assets described in the cardiovascular disease and diabetes chapters are therefore worth considering. Similarly, the assets around wider factors such as poverty and community cohesion, and behaviours such as “tobacco, alcohol, and drug misuse” and “food, obesity and physical activity” are also important to consider. CKD cannot be successfully managed without addressing the common underlying causes.
Given the importance of early diagnosis and management, the nine primary care networks in Kirklees and their constituent services are a vital asset in detecting and commencing management of CKD. Tools such as health checks and blood pressure checks at local pharmacies are already in place to assist in early recognition of CKD. Early and moderate disease is also managed in a primary care setting, as outlined by NICE guidelines (2).
The Kirklees Integrated Wellness Model, the use of population health management, and the move towards personalised care is taking shape in Kirklees. CKD is a multifactorial disease that requires a multi-agency approach to both prevention and treatment, and so this integrated approach is vital.
In Kirklees transplant and renal medicine is provided by the Leeds Renal Service, with outpatient nephrology clinics and nurse-led satellite units in Huddersfield and Dewsbury. These satellite units have capacity for the haemodialysis of 104 established haemodialysis patients. Those starting haemodialysis, peritoneal dialysis, or learning how to carry out home haemodialysis can do so in Leeds.
What significant factors are affecting this issue?
Although many different processes can lead to CKD, the most common by far are high blood pressure and diabetes. In some cases these are preventable conditions, and in many cases with early diagnosis and appropriate management, they are conditions that can be controlled. Well managed, high blood pressure and diabetes are far less likely to cause CKD, or cause existing CKD to progress. The key issues relating to CKD are summarised below:

What does local data tell us?
The prevalence of CKD in Kirklees is just below the national and Yorkshire average, however it still affects over 1 in 20 residents. Further to this, populations in Kirklees such as those of South Asian ethnicity, or from socio-economically deprived areas, are likely to have disproportionately high risk of developing CKD (3).
In North Kirklees, an estimated 80% of those living with CKD have been diagnosed with the condition. In Greater Huddersfield the number is lower, around 60%. Extrapolations from this data suggests that in Kirklees there could be as many as 7000 people with CKD, who are not aware of it (4).
Of those with CKD in Kirklees, around three in four have well controlled blood pressure, this is similar to the national average. Just over three in four have had their urine albumin: creatinine ratio (an important measure of how the kidneys are functioning, recommended by NICE guidelines) measured over a 12 month period, slightly more than the national average (4).
Which groups are affected most by this issue?
Those with high blood pressure and diabetes are most at risk of developing CKD. Inequalities in the distribution of these conditions are discussed in the diabetes and cardiovascular disease chapters. There are further inequalities in risk among the population in Kirklees outlined below (3,5–10).

In order to have equality of outcome there needs to be equity of resource. This ensures at-risk groups are facilitated in taking preventative measures, receive an early diagnosis, and have their high blood pressure, diabetes, and CKD managed appropriately.
Where is this causing greatest concern?
The overall prevalence of CKD in Kirklees is lower than the national and regional average. However some constituent areas of Kirklees have a prevalence higher than the national average. CKD is most prevalent in Mirfield, Batley, Huddersfield, Holmfirth, and Dewsbury (4).

These towns contain some of the region’s most socio-economically deprived areas. This is reflected by compounding risk factors in Dewsbury and Huddersfield especially. In Kirklees the prevalence of diabetes is highest in Batley, Dewsbury, Heckmondwike, and Ashbrow (11). Similar geographical patterns are seen in the variable prevalence of high blood pressure.
Views of local people
The Healthwatch report of West Yorkshire, Harrogate, and Craven involved surveys and focus groups, engaging with nearly 2000 people. With relevance to CKD, the findings highlighted public desire for more prevention of ill health through increased access to check-ups (12).
National surveys of patient renal services reveal the most important factor in determining a patient’s experience is the renal unit where they are treated; patients’ overall experience of the renal services in Leeds (who provide services in Kirklees) is good, and similar to the national average (13). Nationally, patients rate the quality of privacy, dignity and access of services the highest, and rate transport, needling, and decision sharing the lowest.
What could commissioners and service planners consider?
Prevention, early recognition, and prompt, thorough, holistic management of the patient as a whole are vital in reducing the prevalence, morbidity, and mortality of CKD:

References and further information
References
1. Kidney Care UK. Facts and Stats [Internet]. 2019. Available from: https://www.kidneycareuk.org/news-and-campaigns/facts-and-stats/
2. NICE. Chronic Kidney Disease in Adults. 2014.
3. Public Health England. Chronic Kidney Disease Prevalence Estimates. 2014.
4. Public Health England. CVD: Primary Care Intelligence Packs. NHS North Kirklees CCG and Greater HUddersfield CCG. 2017.
5. Luyckx VA, Bertram JF, Brenner BM, Fall C, Hoy WE, Ozanne SE, et al. Effect of fetal and child health on kidney development and long-term risk of hypertension and kidney disease. Lancet. 2013;382(9888):273–83.
6. Yun H-R, Kim H, Park JT, Chang TI, Yoo T-H, Kang S-W, et al. Obesity, metabolic abnormality, and progression of CKD. Am J Kidney Dis. 2018;72(3):400–10.
7. Lightstone L, Rees AJ, Tomson C, Walls J, Winearls CG, Feehally J. High incidence of end-stage renal disease in Indo-Asians in the UK. QJM An Int J Med. 1995;88(3):191–5.
8. Roderick PJ, Raleigh VS, Hallam L, Mallick NP. The need and demand for renal replacement therapy in ethnic minorities in England. J Epidemiol Community Heal. 1996;50(3):334–9.
9. Neugarten J, Golestaneh L. Gender and the prevalence and progression of renal disease. Adv Chronic Kidney Dis. 2013;20(5):390–5.
10. Yacoub R, Habib H, Lahdo A, Al Ali R, Varjabedian L, Atalla G, et al. Association between smoking and chronic kidney disease: a case control study. BMC Public Health. 2010;10(1):731.
11. House of Commons Library. Estimated diabetes prevalence in England. 2017.
12. Healthwatch Leeds. NHS Long Term Plan Summary Report. 2019.
13. Kidney Care UK. A Report on the UK Renal Registry Kidney Care UK Chronic Kidney Disease Patient Reported Experience Measure. 2017.
Further information
More clinical information on CKD can be found in the NHS Health A to Z, available at: https://www.nhs.uk/conditions/kidney-disease/
More information about health checks is available here: https://healthcheck.nhs.uk/
Date this section was last reviewed
19/02/2020 (RJ)
